How will I know if my Medicare drug plan's drug copayments will change next year?
Your Medicare Part D or Medicare Advantage plan coverage can - and probably will change every year. And to see how your Medicare Part D plan will change the plan's cost-sharing (copayment amounts or coinsurance amounts), you can review your plan's Annual Notice of Change (ANOC) letter that your Medicare plan will send you in late-September or early-October of every year.
How can your Medicare prescription drug plan change from year-to-year?
How can your Medicare prescription drug plan change from year-to-year?
- The name of your Medicare Part D plan
- The company that is offering your Medicare Part D plan
- Your monthly premium
- Your annual Initial Deductible
- Your plan's Initial Coverage Limit (when you enter the Donut Hole)
- The quantity and type of drugs that are covered by the plan
- The cost of your drugs - such as the copay when you purchase a formulary drug.
Question: How can I see an overview of all annual Medicare plan changes?
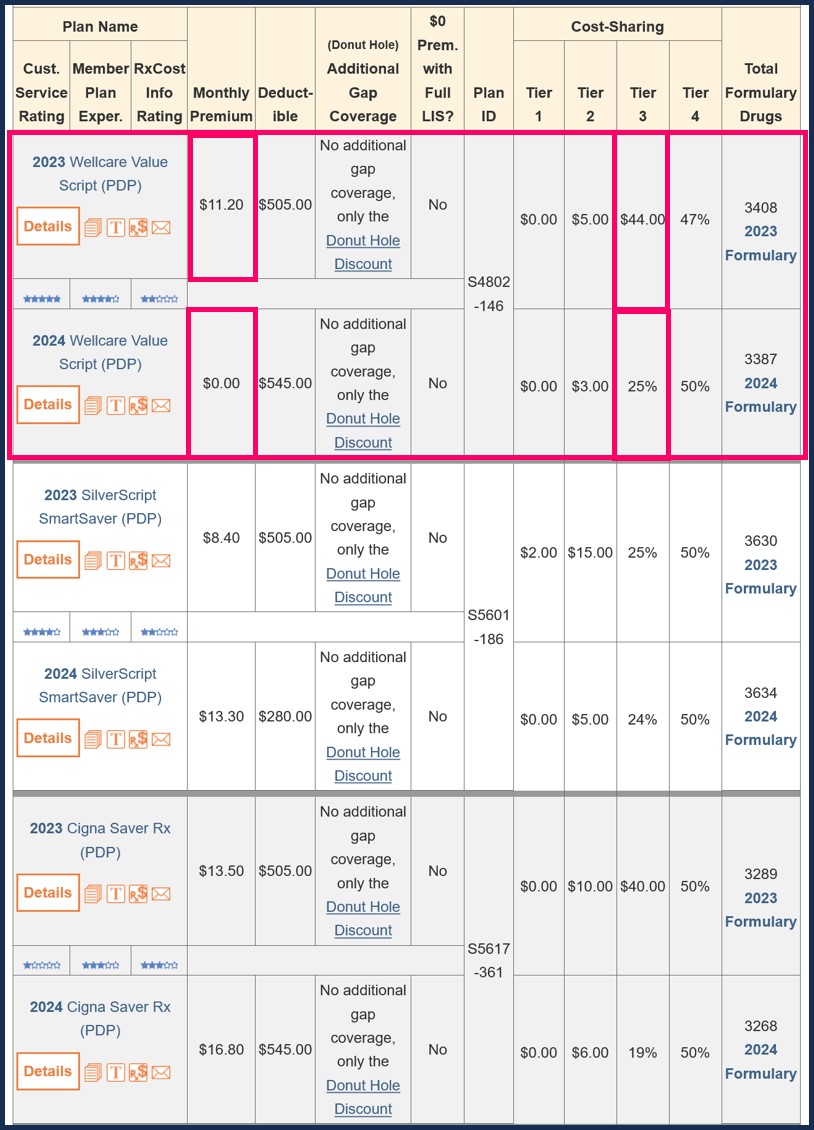
To compare annual changes in Medicare plans, our PDP-Compare and MA-Compare tools show the stand-alone Medicare Part D prescription drug plans (PDPs) and Medicare Advantage plans (MAs or MAPDs) across the country and include changes in plan features such as premium, deductible, cost-sharing and formulary size changes. Our compare tools also highlight plans that were merged, discontinued, or added in the upcoming plan year.
Please also note that copayment amounts may either increase or decrease due to a change in Medicaid eligibility. So, if you no longer qualify for Medicaid or Extra-Help or the Low-Income Subsidy (LIS), you may pay a higher cost sharing for your medications. You can contact your state Medicaid office for more information or telephone Medicare at 1-800-633-4227 to receive assistance from a Medicare representative.
Example: How the Florida Wellcare Value Script changed from 2023 to 2024
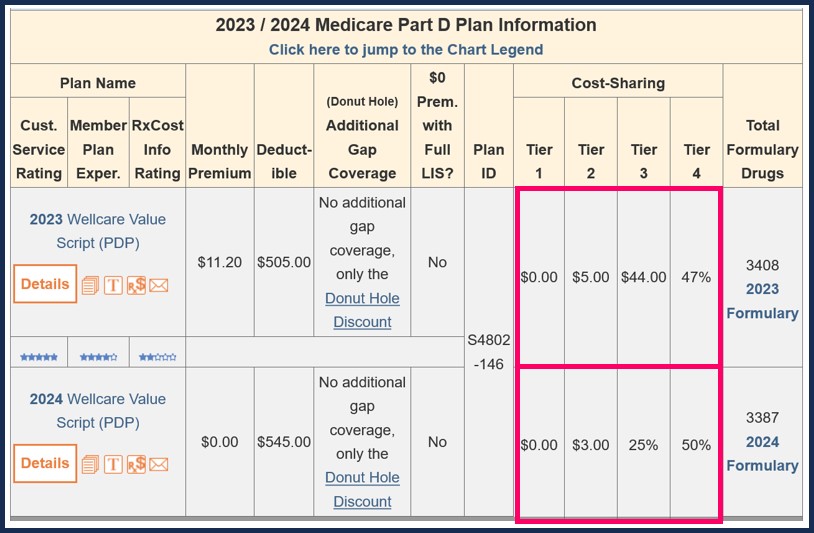
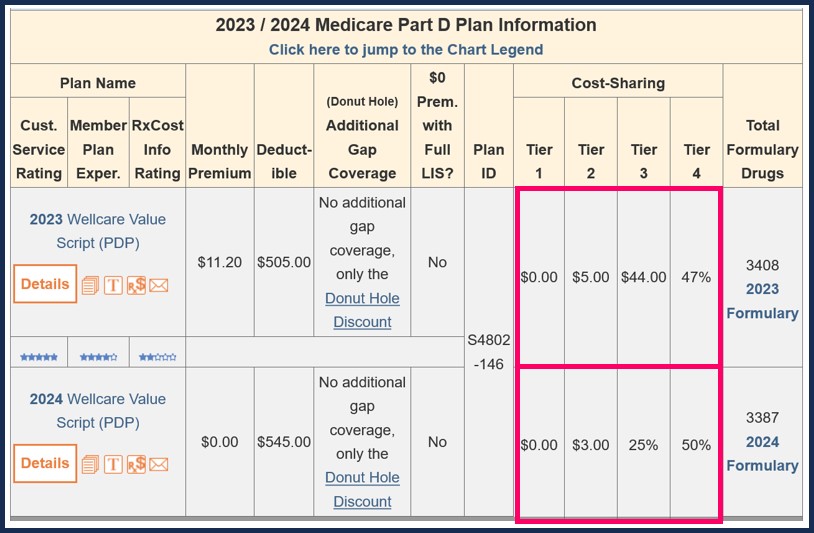
As can be seen in the following example, the 2023 Florida Wellcare Value Script plan formulary covered 1,020 medications as Tier 3 "Preferred Brand" medications (with an $44 copay).
In comparison, the 2024 Florida Wellcare Value Script plan formulary will cover only 960 medications as Tier 3 "Preferred Brand" and these drugs will have a 25% coinsurance.
Here is another view from our Medicare Part D PDP-Compare.com tool (for 2023/2024).
Follow-up Question: Were many people affected by this example of an annual Medicare change?
Yes. Approximately 2,750,000 members in the 2023 Wellcare Value Script plan will see the drug copay changes next year.
In total, over 8.8 million members of various stand-alone Medicare Part D plans will see one or more of the drug tiers change cost-sharing from either coinsurance to copay or copay to coinsurance.
As can be seen in the following example, the 2023 Florida Wellcare Value Script plan formulary covered 1,020 medications as Tier 3 "Preferred Brand" medications (with an $44 copay).
In comparison, the 2024 Florida Wellcare Value Script plan formulary will cover only 960 medications as Tier 3 "Preferred Brand" and these drugs will have a 25% coinsurance.
|
Florida Wellcare Value Script (PDP) 2023 and 2024 Medicare Part D plan Cost-sharing Comparison |
||||||||
| 2023 | 2024 | |||||||
| Monthly Premium | $11.20 | $0.00 | ||||||
| Initial Deductible | $505 | $545 |
||||||
| Gap Coverage | No Gap Coverage | No Gap Coverage | ||||||
Tier |
2023 Cost-Sharing |
Drugs on Tier |
Tier |
2024 Cost-Sharing |
Drugs on Tier |
|||
| 1 | Preferred Generic | $0 | 311 | 1 | Preferred Generic | $0 | 315 | |
| 2 | Generic | $5 | 399 | 2 | Generic | $3 | 387 | |
| 3 | Preferred Brand | $44 | 1,020 | 3 | Preferred Brand | 25% | 960 | |
| 4 | Non-Preferred Drug | 47% | 1,003 | 4 | Non-Preferred Drug | 50% | 1,071 | |
| 5 | Specialty Tier | 25% | 679 | 5 | Specialty Tier | 25% | 601 | |
| 6 | Select Diabetic Drugs | $11 | 42 | 6 | Select Care Drugs | $11 | 53 | |
| Total Formulary Drugs |
Browse 2023 Formulary |
3,408 | Browse 2024 Formulary |
3,387 | ||||
Here is another view from our Medicare Part D PDP-Compare.com tool (for 2023/2024).
Follow-up Question: Were many people affected by this example of an annual Medicare change?
Yes. Approximately 2,750,000 members in the 2023 Wellcare Value Script plan will see the drug copay changes next year.
In total, over 8.8 million members of various stand-alone Medicare Part D plans will see one or more of the drug tiers change cost-sharing from either coinsurance to copay or copay to coinsurance.
Browse FAQ Categories
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
