2025 Medicare Advantage plan Maximum Out-Of-Pocket (MOOP) limits are changing and can reach $9,350 -- with 9.2 million members seeing a MOOP increase from $50 to $6,450.
Your Medicare Advantage plan's Maximum Out-of-Pocket
(MOOP)
threshold limits how much you will
spend on healthcare copayments and coinsurance for eligible Medicare Part A (in-patient
or hospitalization) and Medicare Part B (out-patient or doctor visit) services.
A higher Medicare Advantage MOOP limit means you will spend more out-of-pocket for your Medicare Part A and Medicare Part B covered services before reaching the annual maximum cost threshold.
Each year MOOP limits can change and, in 2025, Medicare Advantage plans can increase the plan's Maximum Out-of-Pocket limit up to $9,350.
Key Points:
Question: How many people will see an increase in their in-network MOOP?
About 9.26 million Medicare Advantage plan members will see an increase in their in-network 2025 MOOP. The MOOP increases for these people can range from $50 to $6,450 - and the following table shows the number of people affected by different ranges of 2025 MOOP increases.
For example, the members of the Humana Gold Plus (HMO) in Verginia will see an increase of $6,450 in the in-network MOOP and members of the Aetna Medicare Premier (HMO-POS) in Arkansas will see a MOOP increase of $4,450.
You can see each Medicare Advantage plan's MOOP using our 2025 Medicare Advantage Plan Finder (MA-Finder.com/2025) or you can browse through the states/counties via our 2025 Overview by State. See annual 2025 Medicare Advantage plan changes such as premium, deductible, MOOP, and formulary size using our MA-Compare tool found at: MA-Compare.com/2025
In-network vs. Out-of-network MOOP
The MOOP limit is a cap on your out-of-pocket expenses and applies to in-network Medicare Part A and Medicare Part B eligible medical cost-sharing. Please refer to your plan's documentation to see whether your out-of-network healthcare costs are included in your MOOP. For example, you may find that local and regional PPO Medicare Advantage plans can have a combined maximum MOOP of up to $14,000 (for in-network and out-of-network coverage) and local HMOs may not include out-of-network healthcare costs in your annual MOOP limit.
The range of in-network 2025 MOOP thresholds
The 2025 Medicare Advantage MOOPs range from $0 to $9,350 — and often, Medicare Advantage plans with a MOOP of $0 are MSAs, or Cost plans. In 2023, Medicare renamed the Voluntary MOOP to "Lower" MOOP and added a third category, "Intermediate" MOOP limit between the two MOOPs -- so the MOOP limits are: "Lower", "Intermediate", and "Mandatory" MOOP.
Question: How are the Lower, Intermediate, and Mandatory MOOP limit set?
The Lower, Intermediate, and Mandatory MOOP limits are set by the Centers for Medicare and Medicaid Services (CMS). Per CMS, the Mandatory MOOP amount represents approximately the 95th percentile of projected beneficiary out-of-pocket spending. In other words, five percent of Original Medicare beneficiaries are expected to incur approximately $9,350 or more in Parts A and B deductibles, copayments, and coinsurance. The Lower MOOP amount of $4,150 represents approximately the 85th percentile of projected Original Medicare out-of-pocket spending. The Intermediate MOOP is set at the numeric midpoint of the Mandatory and Lower MOOP limits.
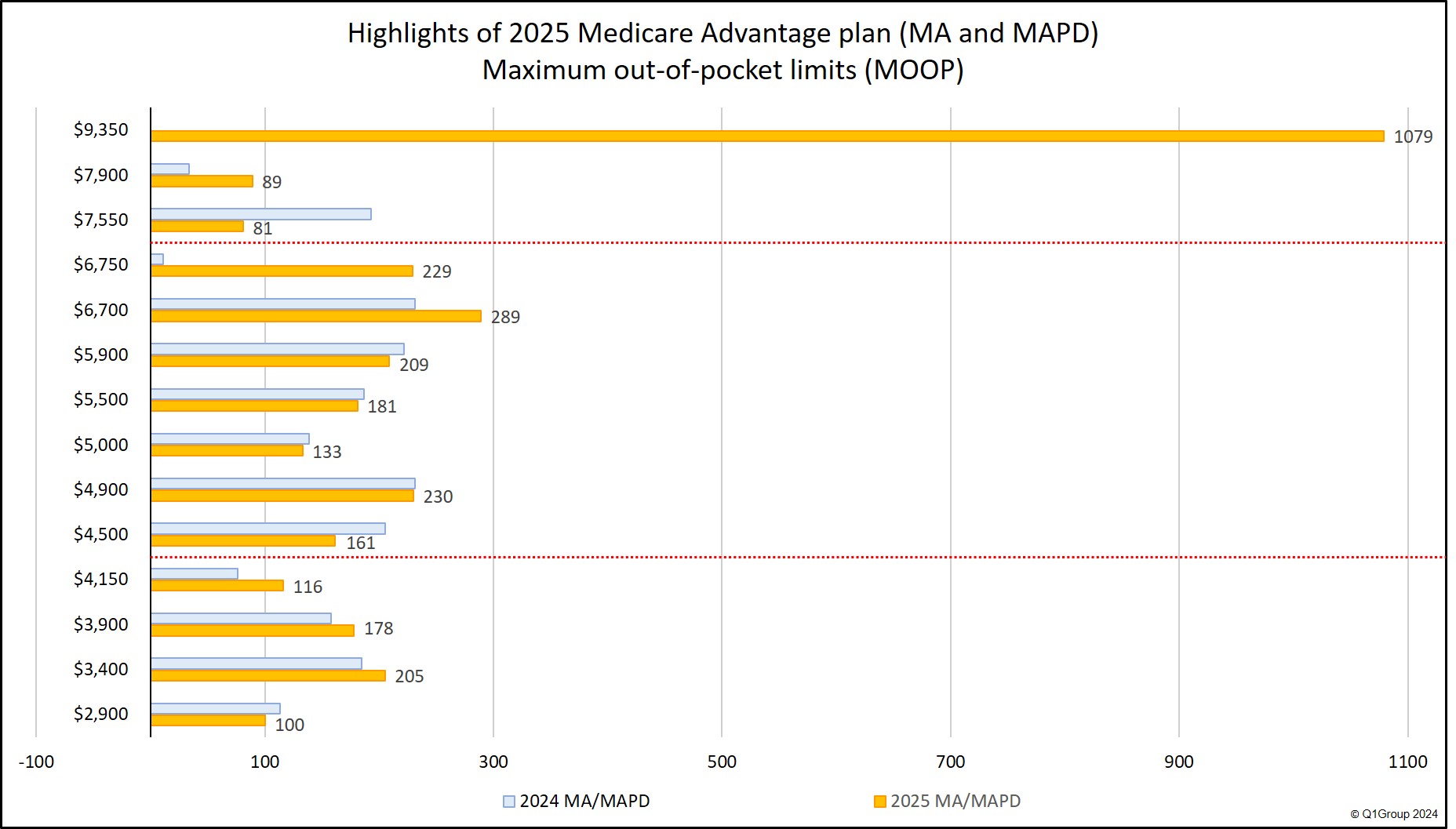
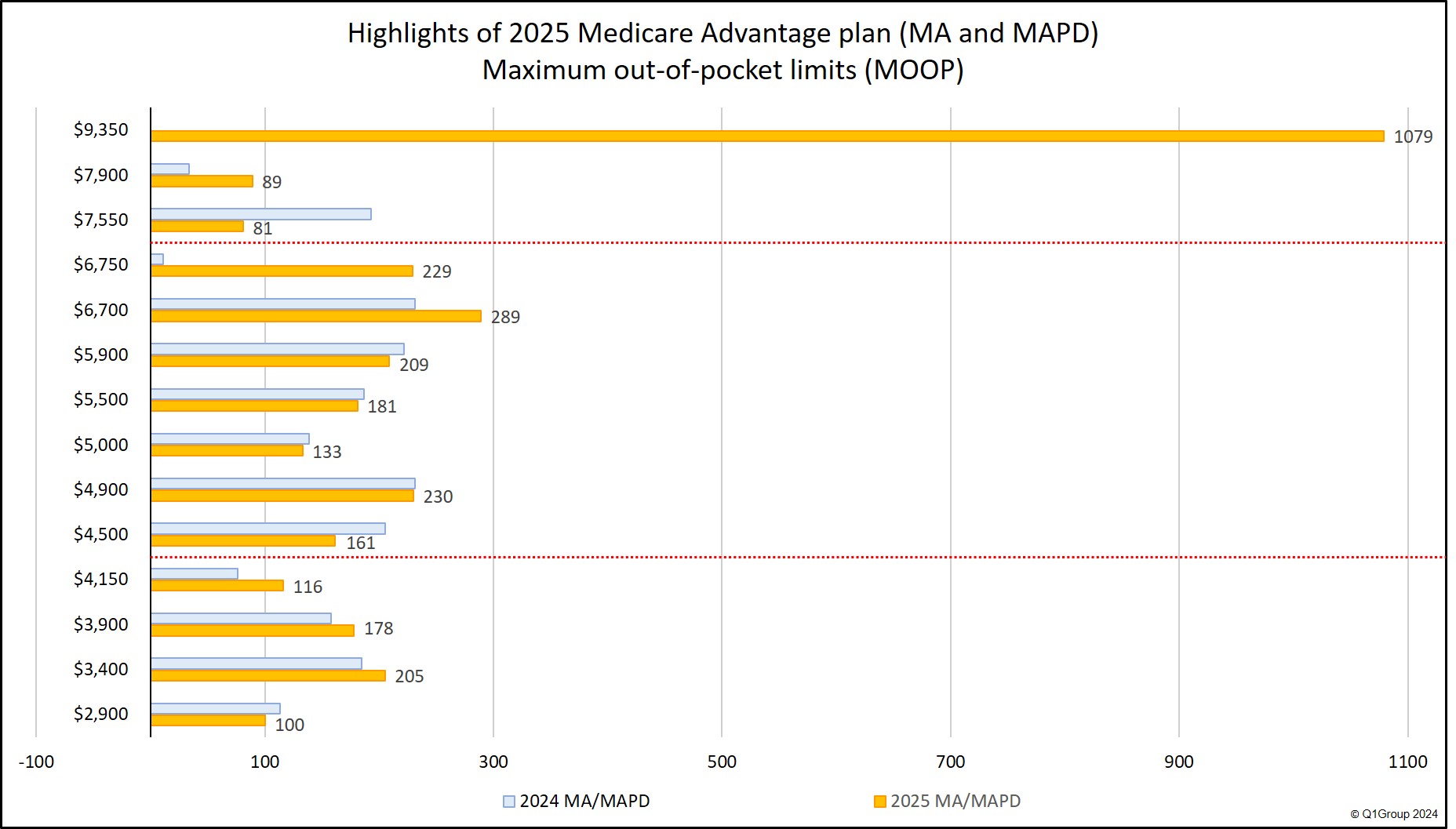
The following chart shows a comparison of the number of plans falling into the three established MOOP ranges.
The following chart highlights the most frequently used 2025 MOOP limits.
The 2025 MOOP dispersion: Different out-of-pocket limits for different Medicare Advantage plans
We found that across all 2025 Medicare Advantage plans, 1,421 plans increased their MOOP, 1,563 plans kept the same MOOP as last year, and 421 plans reduced the plan's MOOP limit.
When MOOP is evaluated across all Medicare Advantage plans (excluding MMPs and SNPs which do not have a MOOP), we see a slight increase in the average 2025 MOOP limit. The 2025 average MOOP is around $5,840 as compared to $5,064 in 2024.
A higher Medicare Advantage MOOP limit means you will spend more out-of-pocket for your Medicare Part A and Medicare Part B covered services before reaching the annual maximum cost threshold.
Each year MOOP limits can change and, in 2025, Medicare Advantage plans can increase the plan's Maximum Out-of-Pocket limit up to $9,350.
Key Points:
- If you have high healthcare expenses, you may want to watch out for an increase in your Medicare Advantage plan's out-of-pocket spending limit.
- If you find that your MOOP is increasing, you may wish to search for another Medicare Advantage plan having a lower MOOP limit ($3,850 or less).
- In short, the higher the MOOP limit, the higher your covered healthcare total expenses can be for the year.
- However, on a positive note, your 2025 Part A and Part B expenses will not exceed $9,350 for in-network Medicare cost-sharing.
- Reminder: MOOP does not include Part D prescription drug expenses or monthly plan premiums.
Question: How many people will see an increase in their in-network MOOP?
About 9.26 million Medicare Advantage plan members will see an increase in their in-network 2025 MOOP. The MOOP increases for these people can range from $50 to $6,450 - and the following table shows the number of people affected by different ranges of 2025 MOOP increases.
2025 Medicare Advantage Plans In-Network MOOP Limit Increases |
|
| Range of MOOP Limit Increase | Number of Members Affected |
| $6,450 | 52,161 |
| $5,000 to $6,449 | 15,099 |
| $4,000 to $4,999 | 30,900 |
| $3,000 to $3,999 | 301,886 |
| $2,000 to $2,999 | 294,640 |
| $1,000 to $1,999 | 1,953,529 |
| $500 to $999 | 2,943,758 |
| less than $500 | 3,653,034 |
For example, the members of the Humana Gold Plus (HMO) in Verginia will see an increase of $6,450 in the in-network MOOP and members of the Aetna Medicare Premier (HMO-POS) in Arkansas will see a MOOP increase of $4,450.
You can see each Medicare Advantage plan's MOOP using our 2025 Medicare Advantage Plan Finder (MA-Finder.com/2025) or you can browse through the states/counties via our 2025 Overview by State. See annual 2025 Medicare Advantage plan changes such as premium, deductible, MOOP, and formulary size using our MA-Compare tool found at: MA-Compare.com/2025
In-network vs. Out-of-network MOOP
The MOOP limit is a cap on your out-of-pocket expenses and applies to in-network Medicare Part A and Medicare Part B eligible medical cost-sharing. Please refer to your plan's documentation to see whether your out-of-network healthcare costs are included in your MOOP. For example, you may find that local and regional PPO Medicare Advantage plans can have a combined maximum MOOP of up to $14,000 (for in-network and out-of-network coverage) and local HMOs may not include out-of-network healthcare costs in your annual MOOP limit.
The range of in-network 2025 MOOP thresholds
The 2025 Medicare Advantage MOOPs range from $0 to $9,350 — and often, Medicare Advantage plans with a MOOP of $0 are MSAs, or Cost plans. In 2023, Medicare renamed the Voluntary MOOP to "Lower" MOOP and added a third category, "Intermediate" MOOP limit between the two MOOPs -- so the MOOP limits are: "Lower", "Intermediate", and "Mandatory" MOOP.
Question: How are the Lower, Intermediate, and Mandatory MOOP limit set?
The Lower, Intermediate, and Mandatory MOOP limits are set by the Centers for Medicare and Medicaid Services (CMS). Per CMS, the Mandatory MOOP amount represents approximately the 95th percentile of projected beneficiary out-of-pocket spending. In other words, five percent of Original Medicare beneficiaries are expected to incur approximately $9,350 or more in Parts A and B deductibles, copayments, and coinsurance. The Lower MOOP amount of $4,150 represents approximately the 85th percentile of projected Original Medicare out-of-pocket spending. The Intermediate MOOP is set at the numeric midpoint of the Mandatory and Lower MOOP limits.
The following chart shows a comparison of the number of plans falling into the three established MOOP ranges.
Medicare Advantage Plans per CMS Defined MOOP Limits |
|||||
| 2025 | 2024 | ||||
| MOOP Limit Range | Nbr of Plans | % of Plans | MOOP Limit Range | Nbr of Plans | % of Plans |
| Lower: $0 to $4,150 |
1,708 | 30% | Lower: $0 to $3,850 | 1,288 | 29% |
| Intermediate: $4,151 to $6,750 |
2,182 | 39% | Intermediate: $3,851 to $6,350 |
2,055 | 46% |
| Mandatory: $6,751 to $9,350 |
1,754 | 31% | Mandatory: $6,351 to $8,850 |
1,057 | 24% |
The following chart highlights the most frequently used 2025 MOOP limits.
The 2025 MOOP dispersion: Different out-of-pocket limits for different Medicare Advantage plans
We found that across all 2025 Medicare Advantage plans, 1,421 plans increased their MOOP, 1,563 plans kept the same MOOP as last year, and 421 plans reduced the plan's MOOP limit.
When MOOP is evaluated across all Medicare Advantage plans (excluding MMPs and SNPs which do not have a MOOP), we see a slight increase in the average 2025 MOOP limit. The 2025 average MOOP is around $5,840 as compared to $5,064 in 2024.
The table below illustrates some of the more frequently occurring 2025 MOOP limits across all types of Medicare Advantage plans. Note that 70% of 2025 Medicare Advantage plans have a MOOP over the $4,150 "Lower" MOOP as compared to 71% over the 2024 "Lower" MOOP of $3,850.
Top 2025 MOOP Limits for Medicare Advantage Plans and statutory Lower, Intermediate, and Mandatory MOOP limits |
||||||
| Number of
Medicare Advantage Plans (MA & MAPD) |
||||||
| MOOP Limits | 2025 | 2024 | Change '24 to '25 | Percent | 2023 | 2022 |
| $9,350 | 1,079 | 0 |
1,079 |
0 |
0 |
|
| $6,700 | 289 | 231 | 58 | 25% | 520 | 520 |
| $4,900 | 230 | 231 | -1 | 0% | 210 | 207 |
| $6,750 | 229 | 11 | 218 | 1,982% | 0 |
0 |
| $5,900 | 209 | 222 | -13 | -6% | 223 | 250 |
| $3,400 | 205 | 185 | 20 | 11% | 207 | 267 |
| $5,500 | 181 | 187 | -6 | -3% | 196 | 186 |
| $3,900 | 178 | 158 | 20 | 13% | 182 | 163 |
| $4,500 | 161 | 205 | -44 | -21% | 206 | 203 |
| $5,000 | 133 | 139 | -6 | -4% | 149 | 134 |
| $4,150 | 116 | 76 | 40 | 53% | 5 | 1 |
| $2,900 | 100 | 113 | -13 | -12% | 122 | 96 |
| $7,900 | 89 | 34 | 55 | 162% | 20 | |
| $7,550 | 81 | 193 | -112 | -58% | 318 | 513 |
| 2025 lower, intermediate, and mandatory MOOP limits | ||||||
| $4,150 | 116 | 76 | 40 | 53% | 5 |
1 |
| $6,750 | 229 | 11 | 218 | 1,982% | 0 |
0 |
| $9,350 | 1,079 | 0 |
1,079 | 0% | 0 |
0 |
The following chart shows how the MOOP range has changed from 2021 through 2025 (excluding $0 MOOP plans).

Medicare Advantage plans may set their MOOP threshold as any amount within the
ranges shown in the CMS table below. As an example, HMO plans can set
their plan's MOOP as high as $9,350. However, an HMO plan that sets MOOP within
the Lower ($0 - $3,850) or Intermediate ($3,851 - $6,350) range is granted greater flexibility for individual
service category cost-sharing.
Important: In-network MOOP and out-of-network MOOP
Again, as can be seen in the table above, out-of-network cost-sharing expenses may fall into a higher MOOP (for example, see Regional PPO above with a higher "combined" MOOP limit) or (IMPORTANT!) your out-of-network cost-sharing may not count toward your MOOP limit, as with the HMO POS plan type. Please notice that the Lower, Intermediate, and Mandatory MOOP limits now change yearly and the 2025 limits are slightly higher than the 2024 figures.
MOOP and Special Needs Plans (and MMPs)
As a reminder, you may notice that Medicare Advantage MMP (Medicare-Medicaid plans) and SNPs (Special Needs Plans), such as SNPs for dual Medicare/Medicaid eligible beneficiaries (D-SNPs), do not have a MOOP.
Reminder about Medicare Advantage MOOP and Part D drug plan TrOOP
Your Total Out-of-Pocket spending limit (TrOOP) for your Medicare Part D prescription drug coverage is not the same as your Medicare Part A and Medicare Part B Maximum Out-of-Pocket spending limit (MOOP). For more information, please see our Frequently Asked Question: TrOOP is not MOOP.
Bottom Line: One of the best features of a Medicare Advantage plan is that, unlike Original Medicare, your annual healthcare spending may be capped at a certain level.
Please review your 2025 Medicare Advantage plan's coverage information to learn more about your plan's MOOP. You should be able to find your 2025 MOOP in your plan's 2025 Annual Notice of Change letter (ANOC). You can also telephone your current Medicare Advantage plan using the toll-free Member Services number found on your Member ID card for more information.
Need additional assistance? Please call Medicare at 1-800-633-4227 and speak with a Medicare representative about Medicare plans that are available in your service area.
You can see more 2025 Medicare Part D plan changes using our MA-Compare tool found at: MA-Compare.com/2025 or Browse Medicare Advantage or Part D plans by state and county.
| 2025 Lower, Intermediate and Mandatory MOOP Range by Type of Medicare Advantage plan |
|||||
| Plan Type | Lower |
Intermediate | Mandatory | ||
| HMO | $0 to $4,150 | $4,151 to $6,750 | $6,751 to $9,350 | ||
| HMO POS | $0 to $4,150 In-network | $4,151 to $6,750 | $6,751 to $9,350 In-network | ||
| Local PPO | $0 to $4,150 In-network and $0 to $6,200 Combined |
$4,151 to $6,750 In-network and $4,151 to $10,100 Combined |
$6,751 to $9,350 In-network and $6,751 to $14,000 Combined |
||
| Regional PPO | $0 to $4,150 In-network and
$0 to $6,200 Combined |
$4,151 to $6,750 In-network and $4,151 to $10,100 Combined |
$6,751 to $9,350 In-network and $6,751 to $14,000 Combined |
||
| PFFS (full network) | $0 to $4,150 | $4,151 to $6,750 | $6,751 to $9,350 Combined | ||
| PFFS (partial network) | $0 to $4,150 | $4,151 to $6,750 | $6,751 to $9,350 Combined | ||
| PFFS (non-network) | $0 to $4,150 | $4,151 to $6,750 | $6,751 to $9,350 | ||
Important: In-network MOOP and out-of-network MOOP
Again, as can be seen in the table above, out-of-network cost-sharing expenses may fall into a higher MOOP (for example, see Regional PPO above with a higher "combined" MOOP limit) or (IMPORTANT!) your out-of-network cost-sharing may not count toward your MOOP limit, as with the HMO POS plan type. Please notice that the Lower, Intermediate, and Mandatory MOOP limits now change yearly and the 2025 limits are slightly higher than the 2024 figures.
MOOP and Special Needs Plans (and MMPs)
As a reminder, you may notice that Medicare Advantage MMP (Medicare-Medicaid plans) and SNPs (Special Needs Plans), such as SNPs for dual Medicare/Medicaid eligible beneficiaries (D-SNPs), do not have a MOOP.
Reminder about Medicare Advantage MOOP and Part D drug plan TrOOP
Your Total Out-of-Pocket spending limit (TrOOP) for your Medicare Part D prescription drug coverage is not the same as your Medicare Part A and Medicare Part B Maximum Out-of-Pocket spending limit (MOOP). For more information, please see our Frequently Asked Question: TrOOP is not MOOP.
Bottom Line: One of the best features of a Medicare Advantage plan is that, unlike Original Medicare, your annual healthcare spending may be capped at a certain level.
Please review your 2025 Medicare Advantage plan's coverage information to learn more about your plan's MOOP. You should be able to find your 2025 MOOP in your plan's 2025 Annual Notice of Change letter (ANOC). You can also telephone your current Medicare Advantage plan using the toll-free Member Services number found on your Member ID card for more information.
Need additional assistance? Please call Medicare at 1-800-633-4227 and speak with a Medicare representative about Medicare plans that are available in your service area.
You can see more 2025 Medicare Part D plan changes using our MA-Compare tool found at: MA-Compare.com/2025 or Browse Medicare Advantage or Part D plans by state and county.
News Categories
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2025 Medicare Part D plan Facts & Figures
- 2025 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2024/2025 Medicare Part D plan changes
- 2025 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2024 to 2025
- Drug Finder: 2025 Medicare Part D drug search
- Formulary Browser: View any 2025 Medicare plan's drug list
- 2025 Browse Drugs By Letter
- Guide to Consumer Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2026 Medicare Part D Reminder Service
