Q1Group 2018 PDP Analysis: Most states will offer fewer 2018 Medicare Part D plans qualifying for the Low-Income Subsidy (LIS) $0 premium
Based on the recently released Centers for Medicare and Medicaid Services (CMS) 2018 Medicare Part D landscape data, on average, fewer 2018 Medicare Part D plans qualify for the Low-Income Subsidy (LIS) $0 premium benchmark as compared to 2017.
The state with the smallest selection of $0-premium LIS plans.
The state offering the smallest selection of 2018 Medicare Part D plans qualifying for the LIS $0 premium is Florida, offering only two (2) $0-premium LIS plans, down from three (3) plans offered in 2017.
As a bit of history . . . back in 2016, Hawaii offered the smallest selection of $0 premium LIS plans with only two (2) qualifying plans (down from 9 plans in 2015). Then in 2017, Hawaii, added three additional Medicare Part D plans qualifying for the $0 premium, increasing the state’s full-LIS $0 qualifying 2017 PDPs to five plan options. In 2018 Hawaii, will lose one (1) Medicare Part D plan qualifying for the $0 premium, decreasing the state’s full-LIS $0 qualifying 2018 PDPs to four.
The states with the largest selection of LIS-qualifying $0 premium Medicare Part D plans is . . .
The states offering the largest selection of ten (10) $0 premium LIS plans in 2018 continue to be : Washington DC, Delaware, Maryland, and Arizona.
In comparison to 2018, in 2015, the states with the largest selection of LIS $0 premium plans were Alabama, Arizona, Idaho, Tennessee, and Utah, all with 12 Medicare Part D plans qualifying for the 2015 LIS $0 premium.
The state with the largest number of LIS recipients is . . .
The state with the most Medicare beneficiaries qualifying for the low-income subsidy is California (almost 1.4 million “Extra Help” recipients). In 2018, California LIS recipients will have five (5) Medicare Part D plan choices qualifying for the $0 premium.
What Medicare Part D plan providers are offering 2018 LIS-qualifying plans?
From our national stand-alone PDP-Facts page, here is a table showing a comparison of the 2017 and 2018 Medicare Part D plans qualifying for the $0 premium Low-Income Subsidy.
Historical changes in the number of LIS-Qualifying Medicare Part D plans
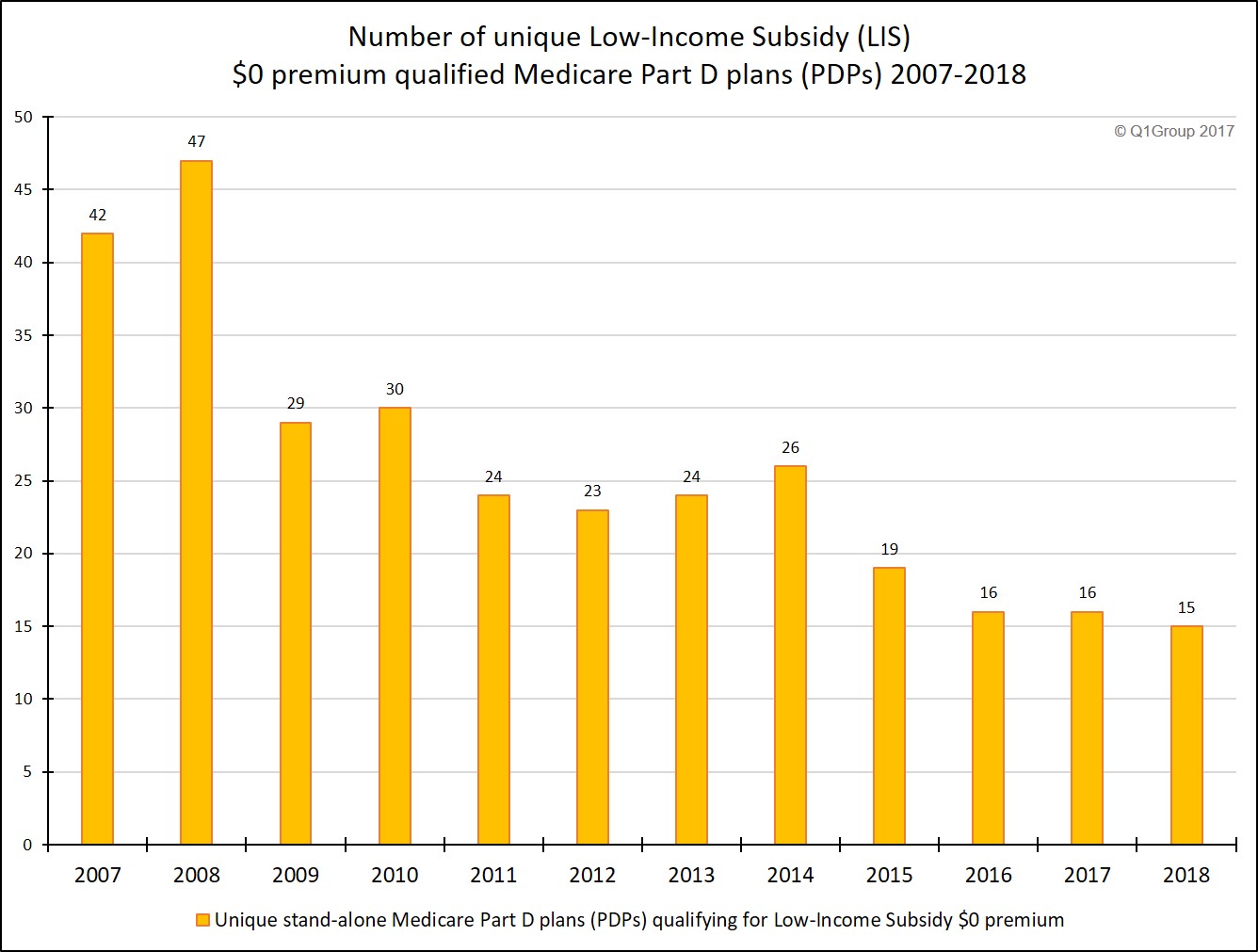
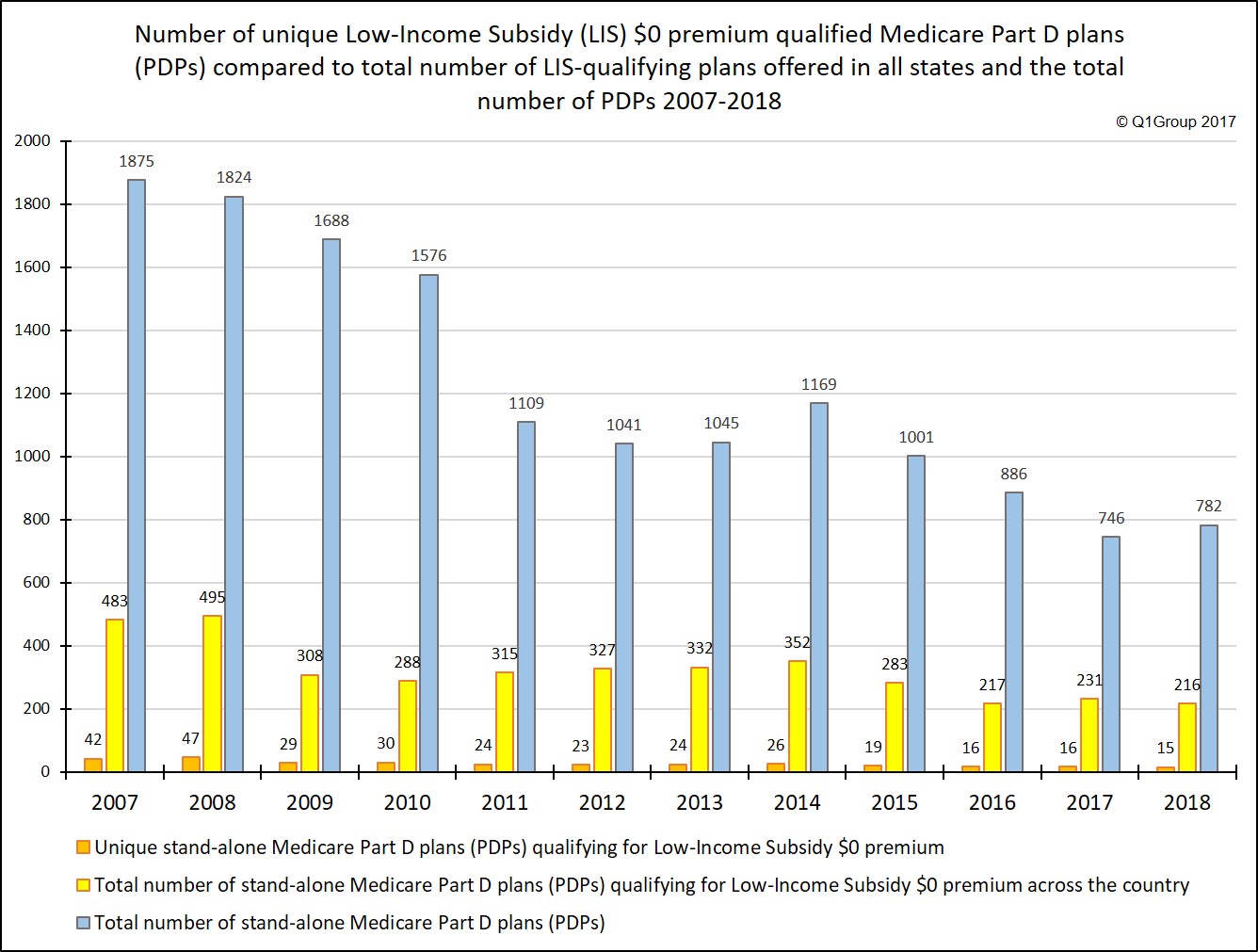
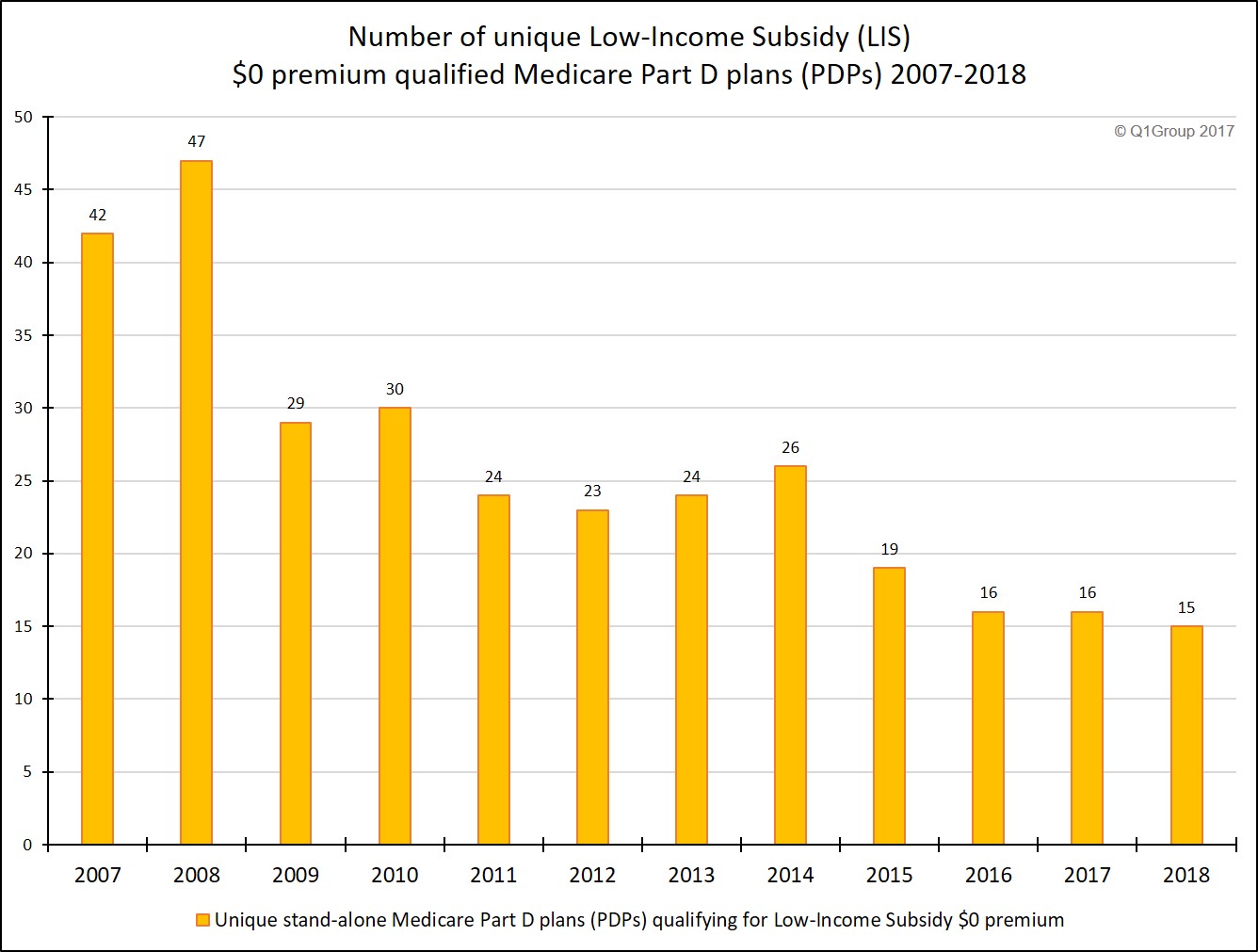
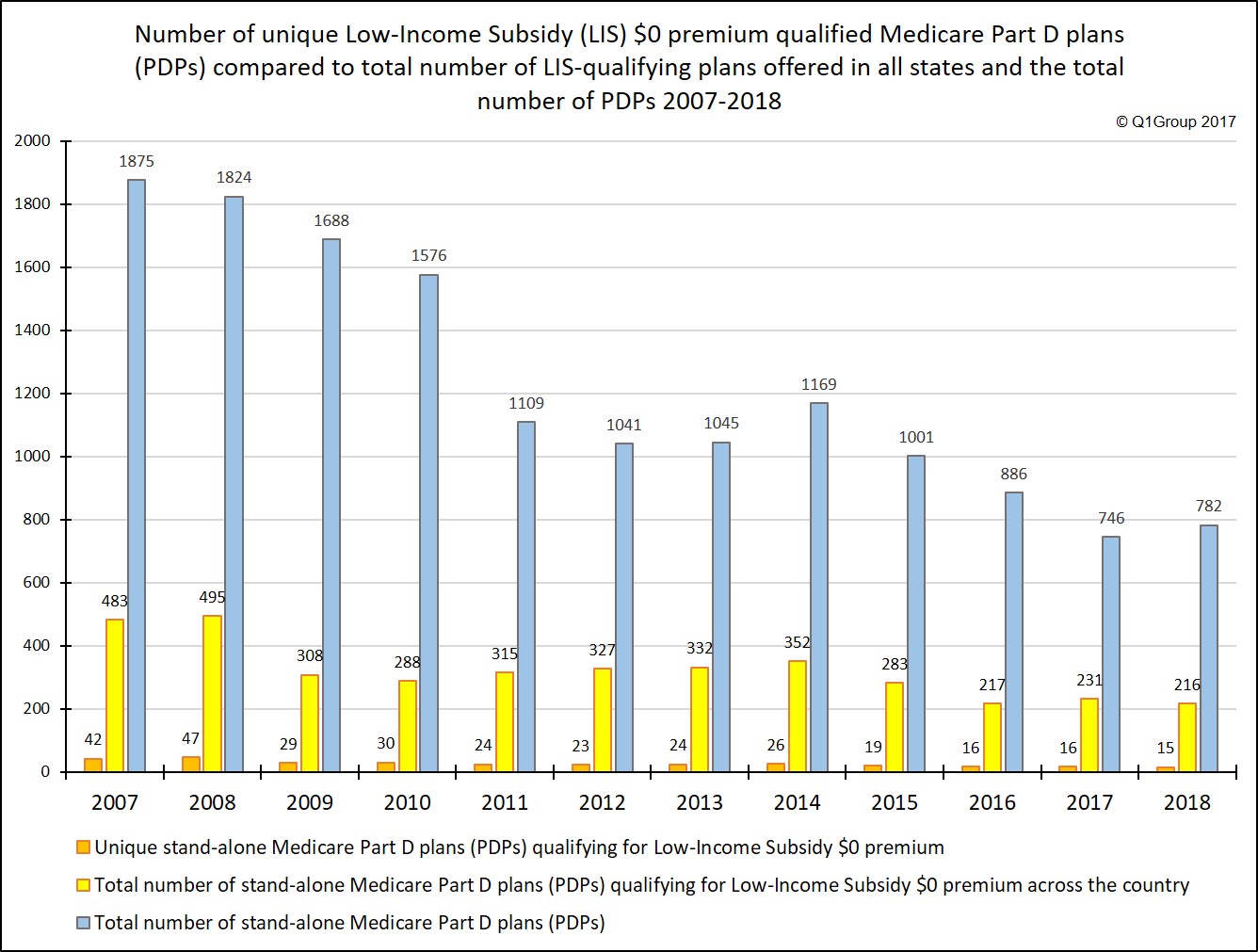
On the positive side, even with fewer LIS-qualifying plans being offered in 2018, the chart below shows that the average number of LIS-qualifying plans has stabilized to some extent over the past several years even as the national stand-alone Medicare Part D landscape has changed.
A few more 2018 LIS $0 premium facts:
Which Medicare Part D plans qualify for the full Low-Income Subsidy $0 premium in your state?
Each year, insurance companies adjust their Medicare Part D plan premiums, and some Medicare Part D plans raise their premiums and move their prescription drug plans above the state low-income subsidy (LIS) benchmark limits, while other Part D plan sponsors lower their monthly premiums so that their plans can qualify for a state’s $0 premium.
This means that the number of Medicare Part D plans qualifying for the LIS $0 premium can change each year. Click on the 2018 premium for your state in our state low-income subsidy (LIS) benchmark limits article to see qualifying plans in your state.
More on Medicare Part D Extra Help
The Medicare Part D Extra Help or the Low-Income Subsidy (LIS) is a federal program helping low-income Medicare beneficiaries pay a portion of their Medicare Part D prescription drug costs. Based on a person’s income and financial resources, the Extra Help or LIS program pays all or part of a person’s monthly Medicare Part D plan premiums and a significant portion of the beneficiary’s medication costs.
If you qualify for the full-LIS program, you can choose a Medicare Part D plan that qualifies for your state’s $0 monthly premium or allow yourself to be automatically enrolled in a plan that qualifies for the $0 premium. If you enroll in a Medicare Part D plan that does not qualify for the $0 premium, you will pay a portion of the premium. The monthly premium amount you will pay is shown under the "Benefit Details" button on our Medicare Part D plan finder.
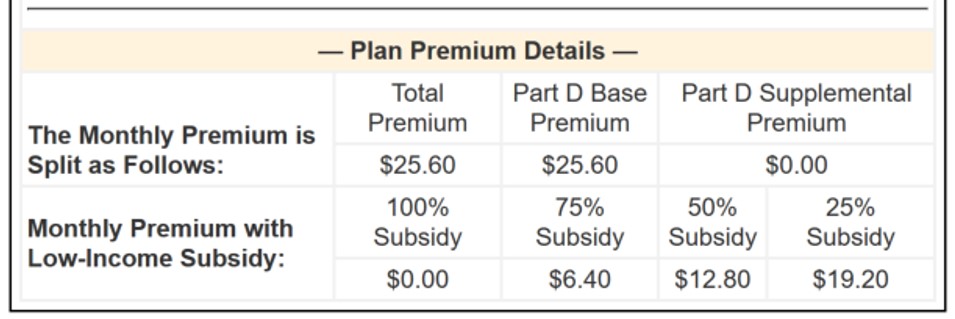
As can be seen in the above graphic, if you qualify for only "partial-LIS benefits" (such as 50% LIS), you will also only pay a portion of the plan's monthly premium.
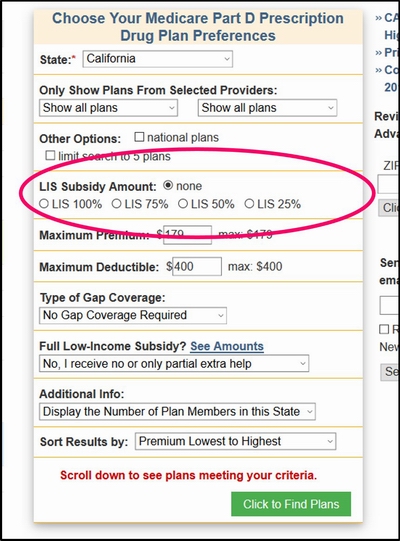
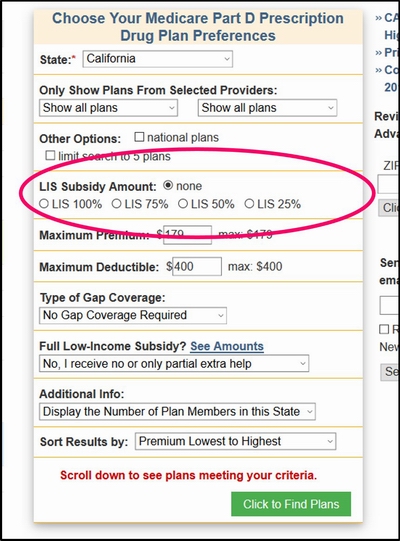
Please note, our Medicare Part D plan finder allows you to view the premiums of a Medicare Part D plan based on whether you receive full - or partial-LIS benefits.
The PDP-Finder.com feature looks like this:
A Brief note about automatic plan reassignment and people who are "choosers"
Because of changes in the annual Medicare Part D plan premiums and state LIS benchmarks, some full low-income subsidy qualifying Medicare beneficiaries (such as people who are Medicare / Medicaid dual-eligible beneficiaries) may be automatically reassigned to new 2017 Medicare Part D plans that will still qualify for the $0 monthly premium.
However, Extra Help recipients who "chose" their own plan in the past (or "choosers") may not be auto-reassigned to a new 2017 LIS qualifying plan and may need to select a new 2018 Medicare Part D plan or Medicare Advantage plan that includes drug coverage that still meets the $0 monthly premium threshold (or pay the small monthly premium). As reference, you can use our PDP-Finder to see LIS qualifying plans in your state. Be sure to select “Yes, show only plans that qualify for $0 premium". Click here to see an example for Texas.
Not sure where to begin?
For more information on Medicare Part D plans that qualify for your state's low-income $0 premium benchmark, please call Medicare toll-free at 1-800-633-4227 and speak with a Medicare representative to learn more about your Medicare Part D and Medicare Advantage plan options.
As an example of state plan changes, Arkansas will offer four (4) LIS $0 premium qualifying 2018 Medicare Part D plans as compared to the five (5) LIS-qualifying plans in 2017 - and 12 LIS-qualifying plans offered way back in 2014.
The state with the smallest selection of $0-premium LIS plans.
The state offering the smallest selection of 2018 Medicare Part D plans qualifying for the LIS $0 premium is Florida, offering only two (2) $0-premium LIS plans, down from three (3) plans offered in 2017.
As a bit of history . . . back in 2016, Hawaii offered the smallest selection of $0 premium LIS plans with only two (2) qualifying plans (down from 9 plans in 2015). Then in 2017, Hawaii, added three additional Medicare Part D plans qualifying for the $0 premium, increasing the state’s full-LIS $0 qualifying 2017 PDPs to five plan options. In 2018 Hawaii, will lose one (1) Medicare Part D plan qualifying for the $0 premium, decreasing the state’s full-LIS $0 qualifying 2018 PDPs to four.
The states with the largest selection of LIS-qualifying $0 premium Medicare Part D plans is . . .
The states offering the largest selection of ten (10) $0 premium LIS plans in 2018 continue to be : Washington DC, Delaware, Maryland, and Arizona.
In comparison to 2018, in 2015, the states with the largest selection of LIS $0 premium plans were Alabama, Arizona, Idaho, Tennessee, and Utah, all with 12 Medicare Part D plans qualifying for the 2015 LIS $0 premium.
The state with the largest number of LIS recipients is . . .
The state with the most Medicare beneficiaries qualifying for the low-income subsidy is California (almost 1.4 million “Extra Help” recipients). In 2018, California LIS recipients will have five (5) Medicare Part D plan choices qualifying for the $0 premium.
What Medicare Part D plan providers are offering 2018 LIS-qualifying plans?
From our national stand-alone PDP-Facts page, here is a table showing a comparison of the 2017 and 2018 Medicare Part D plans qualifying for the $0 premium Low-Income Subsidy.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Note: Click heading above to see plan details in California or choose your state.
Please note, not all plans are available in every state.
Historical changes in the number of LIS-Qualifying Medicare Part D plans
On the positive side, even with fewer LIS-qualifying plans being offered in 2018, the chart below shows that the average number of LIS-qualifying plans has stabilized to some extent over the past several years even as the national stand-alone Medicare Part D landscape has changed.
A few more 2018 LIS $0 premium facts:
- New Mexico and South Carolina are losing two (2) LIS $0 premium plans
- Twenty-Seven (27) states are losing one LIS $0 premium plan
- Seventeen (17) states have no change in the number of LIS $0 premium plans being offered
- Four (4) states are gaining one LIS $0 premium plan
- Alaska is gaining two LIS $0 premium plans
Which Medicare Part D plans qualify for the full Low-Income Subsidy $0 premium in your state?
Each year, insurance companies adjust their Medicare Part D plan premiums, and some Medicare Part D plans raise their premiums and move their prescription drug plans above the state low-income subsidy (LIS) benchmark limits, while other Part D plan sponsors lower their monthly premiums so that their plans can qualify for a state’s $0 premium.
This means that the number of Medicare Part D plans qualifying for the LIS $0 premium can change each year. Click on the 2018 premium for your state in our state low-income subsidy (LIS) benchmark limits article to see qualifying plans in your state.
More on Medicare Part D Extra Help
The Medicare Part D Extra Help or the Low-Income Subsidy (LIS) is a federal program helping low-income Medicare beneficiaries pay a portion of their Medicare Part D prescription drug costs. Based on a person’s income and financial resources, the Extra Help or LIS program pays all or part of a person’s monthly Medicare Part D plan premiums and a significant portion of the beneficiary’s medication costs.
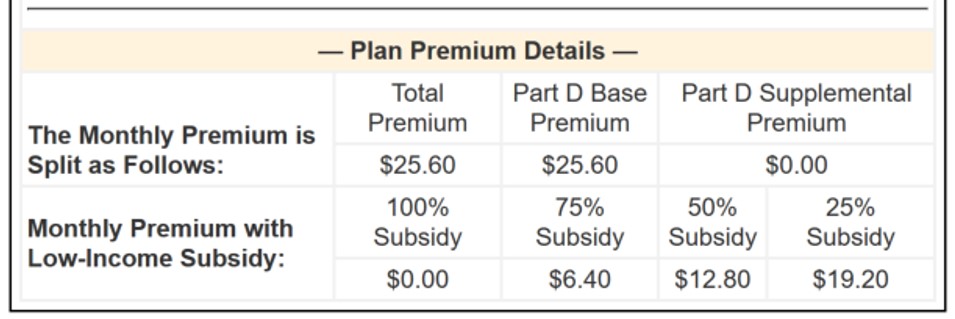
If you qualify for the full-LIS program, you can choose a Medicare Part D plan that qualifies for your state’s $0 monthly premium or allow yourself to be automatically enrolled in a plan that qualifies for the $0 premium. If you enroll in a Medicare Part D plan that does not qualify for the $0 premium, you will pay a portion of the premium. The monthly premium amount you will pay is shown under the "Benefit Details" button on our Medicare Part D plan finder.
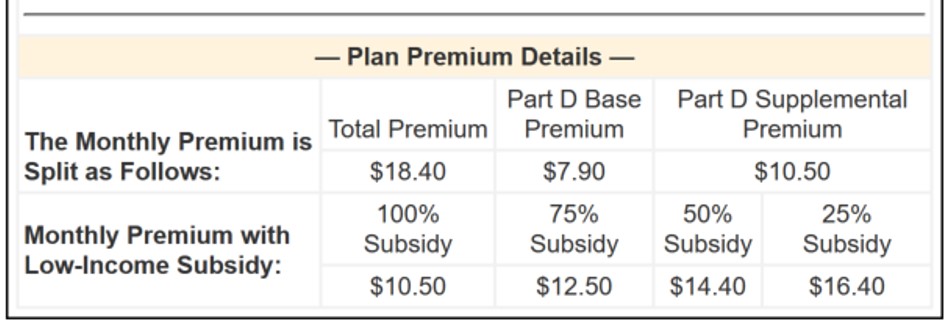
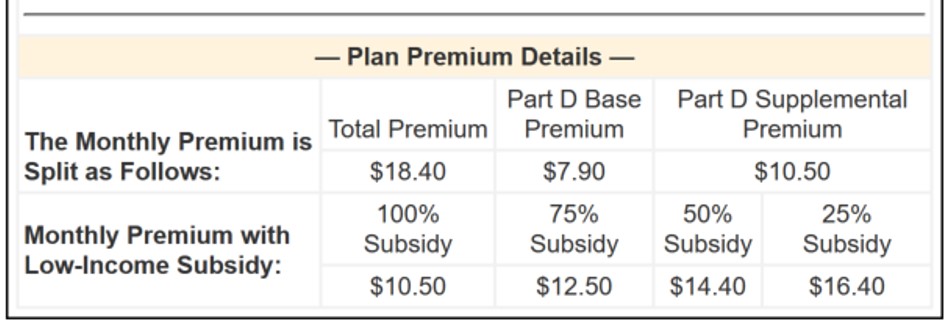
As can be seen in the above graphic, if you qualify for only "partial-LIS benefits" (such as 50% LIS), you will also only pay a portion of the plan's monthly premium.
Please note, our Medicare Part D plan finder allows you to view the premiums of a Medicare Part D plan based on whether you receive full - or partial-LIS benefits.
The PDP-Finder.com feature looks like this:
The applicable monthly premium will be shown in the search results and can be found on our "Benefit Details" page, for example:
A Brief note about automatic plan reassignment and people who are "choosers"
Because of changes in the annual Medicare Part D plan premiums and state LIS benchmarks, some full low-income subsidy qualifying Medicare beneficiaries (such as people who are Medicare / Medicaid dual-eligible beneficiaries) may be automatically reassigned to new 2017 Medicare Part D plans that will still qualify for the $0 monthly premium.
However, Extra Help recipients who "chose" their own plan in the past (or "choosers") may not be auto-reassigned to a new 2017 LIS qualifying plan and may need to select a new 2018 Medicare Part D plan or Medicare Advantage plan that includes drug coverage that still meets the $0 monthly premium threshold (or pay the small monthly premium). As reference, you can use our PDP-Finder to see LIS qualifying plans in your state. Be sure to select “Yes, show only plans that qualify for $0 premium". Click here to see an example for Texas.
Not sure where to begin?
For more information on Medicare Part D plans that qualify for your state's low-income $0 premium benchmark, please call Medicare toll-free at 1-800-633-4227 and speak with a Medicare representative to learn more about your Medicare Part D and Medicare Advantage plan options.
News Categories
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
