(Updated 04/06/2022)
On February 2, 2022, the Centers for Medicare and
Medicaid Services (CMS)
released
the "Advance Notice of Methodological Changes for Calendar Year (CY) 2023 for Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies" (2023 Advance Notice) that included the preliminary defined
standard benefits for
2023 Medicare Part D prescription drug plan coverage and other proposed changes to the Medicare program.
As was expected from the February 2023 Advance Notice, on April 4, 2022, CMS
released the "Announcement of Calendar Year (CY) 2023 Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies (the Rate Announcement)" with the finalized defined standard benefits for 2023 Medicare Part D prescription drug plan coverage as is shown below in more detail. The final defined standard benefits did not vary from the proposed standard benefits published in February.
Why is the Medicare Part D Defined Standard Benefit important?
Each year, CMS publishes the Medicare Part D benefit parameters for the "Defined Standard Benefit" and Medicare Part D plans use this information to determine minimum Part D drug plan coverage for the up-coming plan year.
You can use these same CMS parameters as a preview of how your Medicare
Part D prescription drug plan coverage may change in January 2023 (for example, if you currently pay a $480 deductible, your deductible in 2023 may be $505).
Actual 2023 Medicare Part D plan options and benefit details will be available for your review beginning October
1, 2022 and you can make 2023 plan changes during the fall annual Open Enrollment Period (
AEP) (October 15th through December 7th).
Will all 2023 Medicare Part D prescription drug plans follow these new plan limits?
No. The Medicare Part D defined standard benefit parameters only set minimum standards for next year’s Medicare Part D prescription drug plan coverage. And although some Medicare Part D plans exactly mirror the CMS standard defined benefits, Medicare Part D plans are allowed to deviate from the defined standard benefits and offer Medicare Part D prescription drug plans with
more enhanced features such as offering: a lower or $0 initial deductible (instead of the standard $505 deductible), fixed copays for different drug tiers (instead of a fixed 25% co-insurance), lower
Initial Coverage Limits, or
supplemental drug coverage in the Coverage Gap (in addition to the
Donut Hole discount).
So your actual 2023 Medicare Part D plan may include all - or part of the plan parameters as published in the CMS defined standard benefit - but all Medicare Part D plans are approved by CMS and should provide coverage at least as good, if not better, than the annual defined standard benefits.
How will these changes in 2023 Medicare Part D plan coverage affect you?
Although 2023 Medicare Part D plans are permitted to deviate in structure from the CMS proposed standards and provide even more enhanced coverage, you can still use these proposed CMS figures to approximate your 2023 prescription drug budget - and how your spending will change throughout the plan year. And to assist you with your calculations, you can use our 2023 Donut Hole calculator (found at PDP-Planner.com/2023) to estimate your out-of-pocket spending based on theses CMS standard defined Medicare Part D parameters and your current percentage mix of generic and brand-name drugs. (As a note, based on historical information, CMS is estimating that in 2023, people will use a personal mix of 7.87% generics and 92.13% brand drugs.)
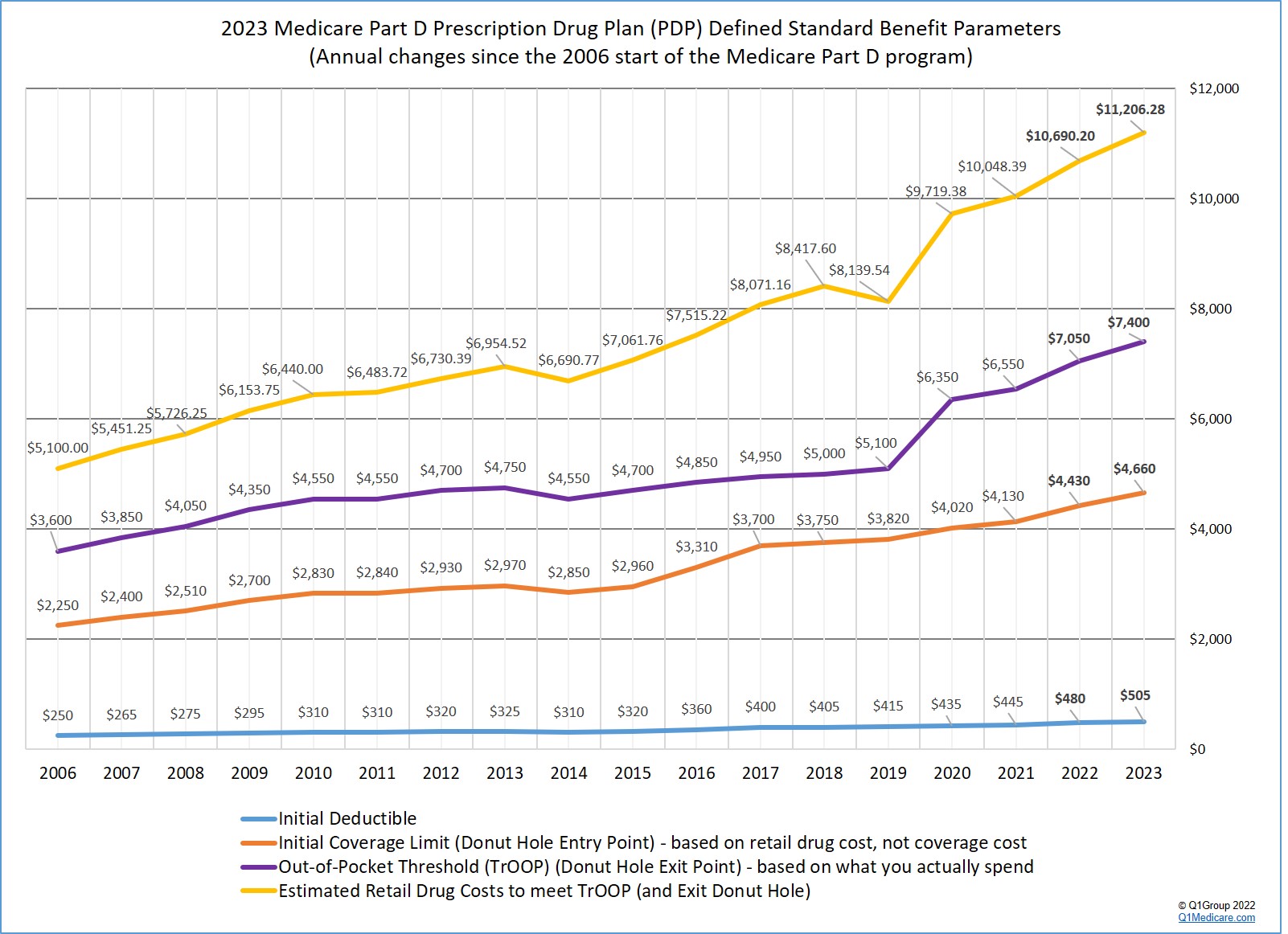
How Medicare Part D plan coverage has changed over the years: As an overview, the following graph shows the 2023 Medicare Part D plan parameters and how standard Medicare Part D plan coverage has changed since the 2006 beginning of the Medicare Part D program. (The Part D information shown is for people who are not eligible for the Medicare Part D Low-Income Subsidy or Extra Help program.)
Based on the 2023 Rate Announcement, here are the "finalized" standard parameters for 2023 Medicare Part D prescription drug coverage:
- The standard 2023 Initial Deductible will increase over 5%.
The 2023 standard Initial Deductible will increase $25 to $505 from the current 2022 standard Initial Deductible of $480. As reference, the 2021 standard Initial Deductible was $445.
What this means to you: The Initial Deductible is the amount that you must pay before your Medicare Part D plan begins to share in the cost of coverage. If you enroll in a Medicare Part D prescription drug plan with a standard Initial Deductible, you will spend slightly more out-of-pocket in 2023 before your plan coverage begins.
As a note, the majority of 2022 Medicare Part D plans have an initial deductible (usually the CMS standard deductible) - and we expect this trend to continue in 2023.
But, as we see in 2022, many popular Medicare Part D plans also exclude lower-costing Tier 1 and Tier 2 drugs from the initial deductible, providing plan Members with immediate coverage for some lower-costing medications.
The Initial Deductible and the Donut Hole: Remember that the Initial Deductible will not affect when you enter the Donut Hole or Coverage Gap, but will impact when you leave the Donut Hole and enter the Catastrophic Coverage portion of your Medicare Part D plan coverage. In other words, what you spend toward your Initial Deductible is counted toward your total out-of-pocket spending threshold or TrOOP (see below for more about TrOOP).
- The Initial Coverage Limit will increase over 5%.
The 2023 Initial Coverage Limit (ICL) will increase $230 to $4,660 from the current 2022 ICL of $4,430 (as reference, the 2021 ICL was $4,130). The Initial Coverage Limit marks the point where you enter the Donut Hole or Coverage Gap. Medicare Part D beneficiaries enter the Donut Hole when the total negotiated retail value of their prescription drug purchases exceeds their plan’s Initial Coverage Limit.
What this means to you: You will need to buy slightly more medications before reaching the 2023 Donut Hole or Coverage Gap (assuming that the retail price of your medications does not increase over time).
- Will you enter the 2023 Donut Hole?
If you purchase medications with an average retail value of over $389 per month (based on your current retail drug prices remaining stable), then you will enter the 2023 Donut Hole at some point during the year. For more information, please see our 2023 Donut Hole calculator to estimate when (or if) you will enter the Donut Hole: PDP-Planner.com/2023
- The 2023 Donut Hole discount for generic drugs remains at 75%.
If you reach the 2023 Donut Hole or Coverage Gap phase of your Medicare Part D plan coverage, the drug discount is 75%. So your generic formulary drug costs in the Donut Hole will be 25% of your plan's negotiated retail prices.
What this means to you: If you are in the 2023 Donut Hole and your generic medication has a retail cost of $100, you will pay only $25 for a refill. And the $25 that you spend for a formulary drug will count toward your 2023 out-of-pocket spending limit or TrOOP of $7,400.
- The Donut Hole discount for brand-name drugs remains at 75%.
The 2023 brand-name drug Donut Hole discount also remains at 75% (you pay 25% of retail costs). The pharmaceutical industry will be responsible for 70% of the cost of medications in the Coverage Gap, therefore you will receive credit for 95% of the retail drug cost toward meeting your 2023 total out-of-pocket maximum or Donut Hole exit point (the 25% of retail costs you pay plus the 70% drug manufacturer discount).
What this means to you: If you reach the 2023 Donut Hole and purchase a brand-name medication with a retail cost of $100, you will pay $25 for the formulary medication, and receive $95 credit toward meeting your 2023 out-of-pocket spending limit – or Donut Hole exit point.
- The amount you need to spend (TrOOP) to exit the 2023 Donut Hole will increase almost 5%
Your 2023 Total Out-of-Pocket Cost (TrOOP) threshold will increase by $350 to $7,400 from the current 2022 TrOOP limit of $7,050. TrOOP is the actual dollar figure you must spend& (or someone else spends on your behalf) to get out of the Donut Hole or Coverage Gap and into the Catastrophic Coverage phase of your Medicare Part D plan and TrOOP does not include monthly premiums or non-formulary purchases. (As reference, the 2021 TrOOP limit was $6,550.)
What this means to you: If you reach the 2023 Donut Hole, you will need to spend slightly more money before exiting the Donut Hole and entering the 2023 Catastrophic Coverage portion of your Medicare Part D plan coverage.
The good news: As noted above, brand-name medication purchases in the 2023 Donut Hole are discounted by 75% (you pay 25%), but you will receive credit of 95% of the retail drug price toward meeting the 2023 TrOOP threshold.
Examples of your prescription purchases needed to meet TrOOP and exit the 2023 Donut Hole:
Example #1: Exiting the Donut Hole with your formulary drug mix is 92.13% brand drugs and 7.87% generic drugs
Using Medicare's past drug usage estimate*, the average person will have purchases of 92.13% brand drugs and 7.87% generic drugs while in the 2023 Donut Hole. So assuming your 2023 Part D plan has a $505 deductible and the retail cost of your drugs is about $934 per month, you can estimate your actual annual out-of-pocket drug costs to be around $3,180 before meeting the $7,400 TrOOP and exiting the 2023 Donut Hole - your Medicare Part D plan would spend about $3,805 and the pharmaceutical manufacturers would spend about $4,220. (As a note, last year, CMS estimated that people in the 2022 Donut Hole would purchase 91.76% brand drugs and 8.24% generic drugs.)
The total retail value of your drug purchases needed to exit the Donut Hole would be around $11,208 (not adjusting for dispensing and vaccine fees). We are also not including your monthly premium costs in this estimate.
Example #2: Exiting the Donut Hole when your formulary drug mix is 100% generics
If you purchase only generic drugs (100% generic) in the Donut Hole - and we assume your Part D has a standard $505 deductible and the retail cost of your drugs is about $2,341 per month, you can expect your estimated annual costs to be $7,400 (or the same as the 2023 TrOOP) before exiting the Donut Hole - your Medicare Part D plan would spend about $20,686 and the pharmaceutical manufacturers would spend $0.
The total retail value of your drug purchases needed to exit the Donut Hole would be $28,092.
Example #3: Exiting the Donut Hole when your Donut Hole drug mix is 100% brand-name
If you purchase only brand drugs (100% brands) - and assuming your Part D plan has a $505 deductible and the retail cost of your drugs is about $903 per month, you can expect your actual annual costs to be around $3,085 before meeting the $7,400 TrOOP and exiting the Donut Hole - your Medicare Part D plan would spend about $3,426 and the pharmaceutical manufacturers would spend about $4,315.
The total retail value of your drug purchases needed to exit the Donut Hole would be $10,836.
What do these examples means to you?
You will spend more out-of-pocket to exit the 2023 Donut Hole as compared to 2022. In fact, the estimated retail value of drug purchases needed to exit the 2023 Donut Hole will increase about 5%. And you would exit the Donut Hole and enter Catastrophic Coverage faster by using brand-name medications in the Donut Hole since the pharmaceutical industry brand-name discount will accelerate you toward meeting your TrOOP.
*CMS estimates that a person will use a mix of 92.13% brand drugs and 7.87% generic drugs while in the 2023 Donut Hole (an increase in estimated brand-name drug use as compared to the 2022 estimated Donut Hole mix of 91.76% brand drugs and 8.24% generic drugs).
Our Donut Hole calculations vs. the CMS cost estimate:
Please note, as shown in the examples above, our estimated cost using our Donut Hole Calculator is slightly different than the CMS total retail drug cost estimate. The variation between our calculations and CMS is because of rounding differences and the consideration of small "dispensing" and "vaccine administration fees" that are being used in the CMS calculation.
Still not sure how the 2023 Donut Hole or Coverage Gap functions?
As noted above, to help you visualize how your current drug spending relates to your Medicare Part D plan coverage, we have our updated 2023 Donut Hole calculator online at: PDP-Planner.com/2023. Our Donut Hole calculator helps you estimate what you can expect to pay throughout the different phases of your 2023 Medicare Part D plan coverage. We have several options for you to choose the percentage of generic and brand drugs you use and you can even change your mix of prescriptions to be 100% generic or 100% brand.
To get you started, you can click here to see an example of the 2023 Medicare prescription drug plan phases for someone with $800 per month brand drug retail cost and has the standard $505 deductible.
(Spoiler alert: If the retail cost of your formulary brand-name medications is $800 per month, you can expect to spend about $2,779 out-of-pocket in 2023 - assuming a $505 deductible and an average brand-name cost-sharing of 25% of retail - and not including monthly premiums).
- Will you exit the Donut Hole and enter the 2023 Catastrophic Coverage phase?
Based on CMS drug purchase estimates, if your monthly retail formulary drug costs are over $389, you will enter the 2023 Donut Hole and if your retail drug costs are over $877 per month, you will exit the 2023 Donut Hole and enter Catastrophic Coverage portion of your Medicare Part D plan.
- 2023 fixed Catastrophic Coverage
costs increase slightly.
The Catastrophic Coverage portion of your Medicare Part D plan begins when you leave the Coverage Gap or Donut Hole. In the 2023 Catastrophic Coverage phase, you pay a minimum of $10.35 for brand drugs or $4.15 for generics (or 5% of retail costs, whichever is higher). As reference, in 2022 Catastrophic Coverage phase, you pay a minimum of $9.85 for brand drugs or $3.95 for generics (or 5%, whichever is higher).
What this means to you: If you purchase a brand name medication with a retail price of over $207 or a generic medication with a retail price of over $83, you will pay 5% of retail or more than the minimum $10.35 for brand drugs or $4.15 for generics.
For example, if you are using the expensive medication IMBRUVICA 140 MG CAPSULE (90 EA) (NDC: 57962014009), your monthly retail drug costs may be over $5,295, so your catastrophic coverage cost would be approximately $265 per month since this 5% of retail cost is more than the minimum $10.35 brand-name catastrophic coverage cost (based on 2022 retail drug costs).
https://www.cms.gov/files/document/2023-advance-notice.pdf
https://www.cms.gov/files/document/2023-announcement.pdf
easy as 1-2-3
- Locate lowest price drug and pharmacy
- Show card at pharmacy
- Get instant savings!
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
