What is the difference between a Medicare Part D standard and preferred network pharmacy?
Potential savings on formulary drug purchases. If you are enrolled in a Medicare Part D prescription drug plan (PDP or MAPD), you will need to visit one of your plan's network pharmacies to receive the cost-saving benefit of your Medicare drug plan. If you visit a non-network pharmacy, you will pay the pharmacy's full retail drug price for the formulary drug.
The good news is that your Medicare drug plan's pharmacy network will include between 50,000 to 60,000 network pharmacies across the country.
However, your Medicare Part D plan can designate some of the plan's network pharmacies as either preferred pharmacies or standard network pharmacies. Each type of network pharmacy can have different cost-sharing and different negotiated retail prices.
In short, as noted by the Centers for Medicare and Medicaid (CMS): "You may pay higher out-of-pocket costs if you get your prescription drugs from a non-preferred pharmacy instead of a preferred [network] pharmacy." But, be sure to look beyond just the cost-sharing at different pharmacies and focus on the total annual cost for your Medicare drug plan to ensure that you have the most economical drug coverage.
How Medicare Part D drug plans have changed their pharmacy networks since 2006.
Although the ability to use both preferred and non-preferred pharmacy cost-sharing has been around since the 2006 beginning of the Medicare Part D program, the use of preferred vs. non-preferred pharmacy cost-sharing really accelerated in 2013.
By 2015, so many Medicare Part D plans were using preferred and non-preferred pharmacies in the plan networks that the term "non-preferred", having a somewhat negative connotation, was replaced with the term "standard" network pharmacy that more closely reflects a network pharmacy's status.
Now, almost all stand-alone Medicare prescription drug plans (PDPs) use preferred and standard network pharmacy pricing as compared to having all pharmacies using a single pricing and cost-sharing structure (for example, in 2024, 93% of all Medicare PDPs use the standard and preferred network pharmacy structure).
The "preferred" or "standard" network pharmacy designation can apply to both retail and mail-order pharmacies. So there can be four (4) different cost-sharing structures depending on your particular prescription (30-day, 60-day, 90-day):
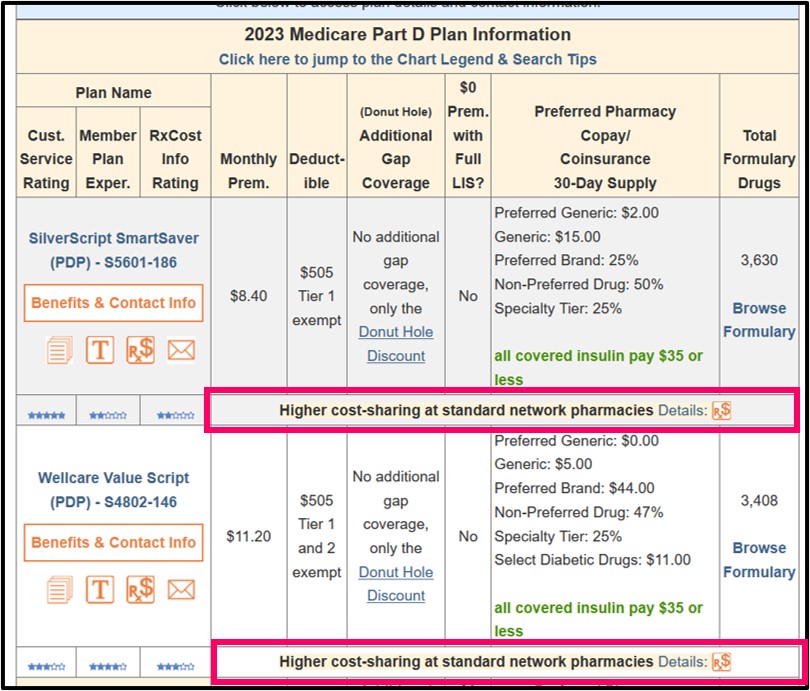
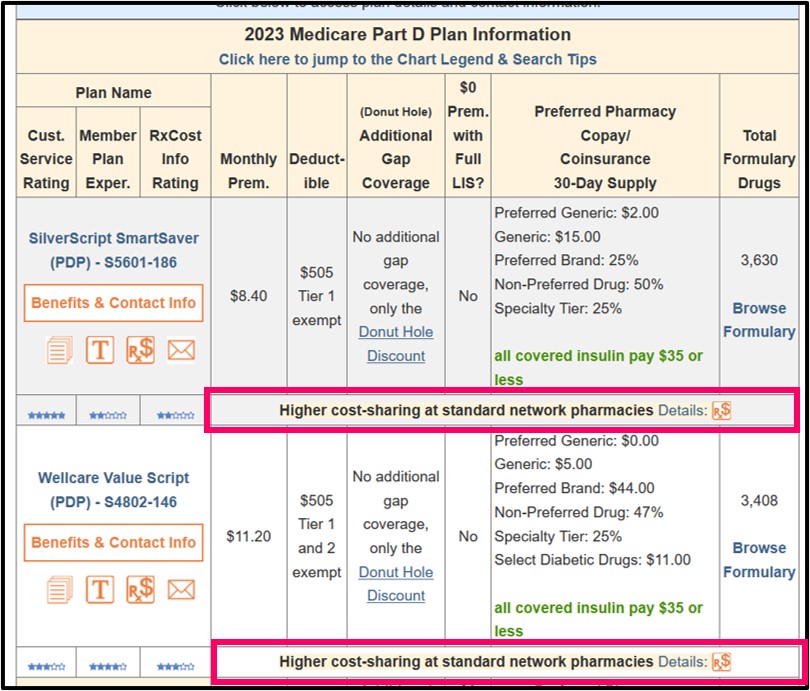
Both our PDP-Finder and MA-Finder show the note: "Higher cost-sharing at standard network pharmacies" if a drug plan uses preferred network pharmacy pricing – and again, this means the cost-sharing you pay is different depending on whether you purchase your medications from a preferred network pharmacy or a standard network pharmacy. You can also see an "Rx$" icon after this note and a "Details" link showing you more information about preferred vs. standard cost-sharing for the chosen Medicare Part D plan.
Our Q1Medicare Formulary Browser (Formulary-Browser.com) and Drug Finder (Q1Rx.com) tools also include the icon with a link to the plan's cost-sharing details, where you can see the following:
icon with a link to the plan's cost-sharing details, where you can see the following:
Question: How do I know which specific pharmacies in my area have preferred or standard cost-sharing for our Medicare drug plan?
First, your Medicare Part D plan documentation (Summary of Benefits and Evidence of Coverage) should tell you whether your Medicare Part D plan has preferred cost-sharing. Look for text in your Evidence of Coverage document such as:
(1) Refer to your Medicare drug plan's pharmacy directory.
You might have also received a printed Pharmacy Directory that will tell you more about preferred / standard pharmacies in your area. If you did not receive a printed pharmacy directory, call your Medicare drug plan's Member Services department using the toll-free number found on your member ID card and ask to be sent a pharmacy directory. If you do not want a printed copy of the pharmacy directory, you can download an electronic version of the pharmacy document from your plan's website.
(2) Use your plan's online Pharmacy locator.
Medicare Part D plans also usually have an easily accessible online pharmacy search tool that allows you to search for network pharmacies in your area and indicates which pharmacies have preferred or standard network cost-sharing.
(3) Call your plan and ask for assistance.
If you cannot find your plan's online pharmacy search, you can call your Medicare plan's Member Services toll-free number (found on enrollment information, printed plan information, and your Member ID card) and ask a Member Services representative to help you find a preferred pharmacy in your area (especially if you are traveling to another area).
The good news is that your Medicare drug plan's pharmacy network will include between 50,000 to 60,000 network pharmacies across the country.
However, your Medicare Part D plan can designate some of the plan's network pharmacies as either preferred pharmacies or standard network pharmacies. Each type of network pharmacy can have different cost-sharing and different negotiated retail prices.
In short, as noted by the Centers for Medicare and Medicaid (CMS): "You may pay higher out-of-pocket costs if you get your prescription drugs from a non-preferred pharmacy instead of a preferred [network] pharmacy." But, be sure to look beyond just the cost-sharing at different pharmacies and focus on the total annual cost for your Medicare drug plan to ensure that you have the most economical drug coverage.
How Medicare Part D drug plans have changed their pharmacy networks since 2006.
Although the ability to use both preferred and non-preferred pharmacy cost-sharing has been around since the 2006 beginning of the Medicare Part D program, the use of preferred vs. non-preferred pharmacy cost-sharing really accelerated in 2013.
By 2015, so many Medicare Part D plans were using preferred and non-preferred pharmacies in the plan networks that the term "non-preferred", having a somewhat negative connotation, was replaced with the term "standard" network pharmacy that more closely reflects a network pharmacy's status.
Now, almost all stand-alone Medicare prescription drug plans (PDPs) use preferred and standard network pharmacy pricing as compared to having all pharmacies using a single pricing and cost-sharing structure (for example, in 2024, 93% of all Medicare PDPs use the standard and preferred network pharmacy structure).
The "preferred" or "standard" network pharmacy designation can apply to both retail and mail-order pharmacies. So there can be four (4) different cost-sharing structures depending on your particular prescription (30-day, 60-day, 90-day):
- "Preferred" retail pharmacies,
- "Standard" (non-preferred) retail pharmacies,
- "Preferred" mail-order pharmacies, and
- "Standard" (non-preferred) mail-order pharmacies.
Both our PDP-Finder and MA-Finder show the note: "Higher cost-sharing at standard network pharmacies" if a drug plan uses preferred network pharmacy pricing – and again, this means the cost-sharing you pay is different depending on whether you purchase your medications from a preferred network pharmacy or a standard network pharmacy. You can also see an "Rx$" icon after this note and a "Details" link showing you more information about preferred vs. standard cost-sharing for the chosen Medicare Part D plan.
Our Q1Medicare Formulary Browser (Formulary-Browser.com) and Drug Finder (Q1Rx.com) tools also include the
- 30-Day preferred retail pharmacy cost-sharing,
- 30-Day standard (non-preferred) retail pharmacy cost-sharing,
- 30-Day preferred mail-order pharmacy cost-sharing,
- 90-Day preferred retail pharmacy cost-sharing,
- 90-Day standard (non-preferred) retail pharmacy cost-sharing,
- 90-Day preferred mail-order pharmacy cost-sharing,
Question: How do I know which specific pharmacies in my area have preferred or standard cost-sharing for our Medicare drug plan?
First, your Medicare Part D plan documentation (Summary of Benefits and Evidence of Coverage) should tell you whether your Medicare Part D plan has preferred cost-sharing. Look for text in your Evidence of Coverage document such as:
"The Pharmacy Directory will also tell you which of the pharmacies in our network have preferred cost-sharing, which may be lower than the standard cost-sharing offered by other network pharmacies."To find a preferred network pharmacy in your area with (probably) the best drug prices:
(1) Refer to your Medicare drug plan's pharmacy directory.
You might have also received a printed Pharmacy Directory that will tell you more about preferred / standard pharmacies in your area. If you did not receive a printed pharmacy directory, call your Medicare drug plan's Member Services department using the toll-free number found on your member ID card and ask to be sent a pharmacy directory. If you do not want a printed copy of the pharmacy directory, you can download an electronic version of the pharmacy document from your plan's website.
(2) Use your plan's online Pharmacy locator.
Medicare Part D plans also usually have an easily accessible online pharmacy search tool that allows you to search for network pharmacies in your area and indicates which pharmacies have preferred or standard network cost-sharing.
(3) Call your plan and ask for assistance.
If you cannot find your plan's online pharmacy search, you can call your Medicare plan's Member Services toll-free number (found on enrollment information, printed plan information, and your Member ID card) and ask a Member Services representative to help you find a preferred pharmacy in your area (especially if you are traveling to another area).
Question: How about an example showing how preferred and standard network pharmacy copayments compare?
As an example of different cost-sharing between network pharmacies, the chart below shows the variation between preferred and standard network pharmacies for the 2024 California SilverScript Choice (PDP) plan (please note that copayments can change year-to-year).
| California SilverScript Choice (S5601-064) | ||||||
| 30-Day Supply Cost-Sharing | 90-Day Supply Cost-Sharing | |||||
| Preferred Pharmacy | Standard Pharmacy |
Preferred Mail-Order |
Preferred Pharmacy | Standard Pharmacy |
Preferred Mail-Order |
|
| Initial Coverage Phase Cost-Sharing (before Donut Hole) |
||||||
| Tier 1 - Preferred Generic: | $2.00 | $8.00 | $2.00 | $6.00 | $24.00 | $6.00 |
| Tier 2 - Generic: | $7.00 | $15.00 | $7.00 | $21.00 | $45.00 | $21.00 |
| Tier 3 - Preferred Brand: | 16% | 16% | 16% | 16% | 16% | 16% |
| Tier 4 - Non-Preferred Brand: | 36% | 36% | 36% | 36% | 36% | 36% |
| Tier 5 - Specialty Tier: | 25% | 25% | 25% | n/a | n/a | n/a |
Remember: Preferred and standard network pharmacy cost-sharing shown above can vary by state.
As a second example, the chart below shows the variation between preferred and standard network pharmacies for the 2024 WellCare Classic plan.
| Texas WellCare Classic (PDP) (S4802-013) | ||||||
| 30-Day Supply Cost-Sharing | 90-Day Supply Cost-Sharing | |||||
| Preferred Pharmacy | Standard Pharmacy |
Preferred Mail-Order |
Preferred Pharmacy | Standard Pharmacy |
Preferred Mail-Order |
|
| Initial Coverage Phase Cost-Sharing | ||||||
| Tier 1 - Preferred Generic: | $0.00 | $3.00 | $0.00 | $0.00 | $9.00 | $0.00 |
| Tier 2 - Generic: | $5.00 | $8.00 | $5.00 | $15.00 | $24.00 | $15.00 |
| Tier 3 - Preferred Brand: | 22% | 22% | 22% | 22% | 22% | 22% |
| Tier 4 - Non-Preferred Brand: | 42% | 42% | 42% | 42% | 42% | 42% |
| Tier 5 - Specialty Tier: | 25% | 25% | 25% | n/a | n/a | n/a |
Note: Again, the preferred and standard network pharmacy cost-sharing shown above can vary by state.
Question: How about an actual example of how formulary drug costs can vary between preferred and standard pharmacies?
As an example of how the different cost-sharing could affect your prescription drug spending, the chart below shows how the total prescription costs for three medications (Atorvastatin, Clopidogrel, and Esomeprazole Magnesium) can vary between different network pharmacies (such as CVS, Walmart, or Walgreens), depending on your Medicare Part D plan.
You will notice in the example that sometimes these example pharmacies will be preferred network (P) or standard network (S) and that the total cost illustrates the difference in the plan's negotiated retail drug price for all three prescriptions combined. The first example is drug cost along (not considering the plan premium) and the second example includes the same analysis including the plan's monthly premium.
Spoiler Alert: You may pay more for your medications at a standard network pharmacy (but not always!) — and you may pay a whole lot more for medications at a non-network pharmacy.
*Annual Drug Cost Estimates from Medicare.gov Plan Finder 10/22/2023 less the annual premium.
(P) Preferred network pharmacy pricing for the designated Medicare Part D plan
(S) Standard network pharmacy pricing for the designated Medicare Part D plan
**Annual Drug Cost Estimates from Medicare.gov Plan Finder 10/22/2023.
(P) Preferred network pharmacy pricing for the designated Medicare Part D plan
(S) Standard network pharmacy pricing for the designated Medicare Part D plan
Bottom Line: Consider Preferred v. Standard cost-sharing, Retail drug costs, and Total annual plan cost.
If you want to lower your prescription drug costs, make sure you are using one of your plan’s preferred network pharmacies (or preferred mail order option). HOWEVER, as noted in the charts above, it can happen that the retail prices at a standard network pharmacy may be lower and your plan's coinsurance is not significantly different between preferred and standard network pharmacies. Plus, you must consider both the coverage cost of your prescriptions at a network pharmacy and the cost of the plan's monthly premium to determine which Medicare Part D plan provides the most economical coverage.
As an example of how the different cost-sharing could affect your prescription drug spending, the chart below shows how the total prescription costs for three medications (Atorvastatin, Clopidogrel, and Esomeprazole Magnesium) can vary between different network pharmacies (such as CVS, Walmart, or Walgreens), depending on your Medicare Part D plan.
You will notice in the example that sometimes these example pharmacies will be preferred network (P) or standard network (S) and that the total cost illustrates the difference in the plan's negotiated retail drug price for all three prescriptions combined. The first example is drug cost along (not considering the plan premium) and the second example includes the same analysis including the plan's monthly premium.
Spoiler Alert: You may pay more for your medications at a standard network pharmacy (but not always!) — and you may pay a whole lot more for medications at a non-network pharmacy.
| 2024 Medicare Part D Drug Costs Only Without including plan premiums |
||||
| 2024 Medicare Part D Plan Name | Annual Cost at CVS* | Annual Cost at Walmart* | Annual Cost at Walgreens* | Annual Cost Preferred Mail Order* |
| Cigna Saver Rx (PDP) | $513.00 (S) | $276.60 (P) | $249.12 (P) | $288.00 (P) |
| Humana Walmart Value Rx Plan (PDP) | $162.00 (S) | $82.80 (P) | $174.60 (S) | $92.40 (P) |
| AARP MedicareRx Walgreens (PDP) | $612.00 (S) | $612.00 (S) | $77.28 (P) | $77.24 (P) |
| SilverScript Plus | $0 (P) | $0 (P) | $55.56 (S) | $0 (P) |
| WellCare Value Script | $1,370.25 (P) | $1,625.00 (S) | $1.464.46 (P) | $1,510.90 (P) |
| Mutual of Omaha Rx Essential | $103.80 (P) | $175.80 (P) | $175.32 (S) | $129.60 (P) |
*Annual Drug Cost Estimates from Medicare.gov Plan Finder 10/22/2023 less the annual premium.
(P) Preferred network pharmacy pricing for the designated Medicare Part D plan
(S) Standard network pharmacy pricing for the designated Medicare Part D plan
| 2024 Medicare Part D Drug Costs With plan premiums included with the drug costs |
||||
| 2024 Medicare Part D Plan Name | Annual Cost at CVS** | Annual Cost at Walmart** | Annual Cost at Walgreens** | Annual Cost Preferred Mail Order** |
| Cigna Saver Rx (PDP) | $743.40 (S) | $507.00 (P) | $479.52 (P) | $518.40 (P) |
| Humana Walmart Value Rx Plan (PDP) | $642.00 (S) | $562.80 (P) | $654.60 (S) | $572.40 (P) |
| AARP MedicareRx Walgreens (PDP) | $1,262.40 (S) | $1,262.40 (S) | $727.68 (P) | $727.64 (P) |
| SilverScript Plus | $1,213.20 (P) | $1,213.20 (P) | $1,268.76 (S) | $1,213.20 (P) |
| WellCare Value Script | $1,370.25 (P) | $1,625.00 (S) | $1,464.46 (P) | $1,510.90 (P) |
| Mutual of Omaha Rx Essential | $393.00 (P) | $465.00 (P) | $464.52 (S) | $418.80 (P) |
(P) Preferred network pharmacy pricing for the designated Medicare Part D plan
(S) Standard network pharmacy pricing for the designated Medicare Part D plan
Bottom Line: Consider Preferred v. Standard cost-sharing, Retail drug costs, and Total annual plan cost.
If you want to lower your prescription drug costs, make sure you are using one of your plan’s preferred network pharmacies (or preferred mail order option). HOWEVER, as noted in the charts above, it can happen that the retail prices at a standard network pharmacy may be lower and your plan's coinsurance is not significantly different between preferred and standard network pharmacies. Plus, you must consider both the coverage cost of your prescriptions at a network pharmacy and the cost of the plan's monthly premium to determine which Medicare Part D plan provides the most economical coverage.
Browse FAQ Categories
Compare Local Pharmacy Prices Using a Drug Discount Card
Prescription Discounts are
easy as 1-2-3
easy as 1-2-3
- Locate lowest price drug and pharmacy
- Show card at pharmacy
- Get instant savings!
Your drug discount card is available to you at no cost.
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
