What is my Medicare Part D plan's Initial Coverage Phase?
The Initial Coverage phase is the second part of your Medicare Part D drug plan and follows the Initial Deductible (if your plan has a deductible). During this phase, you and your Medicare Part D plan share in the cost of your formulary drugs (for example, you pay $47 for a $500 drug).
As a review, 2025 Medicare Part D prescription drug plans have three different parts of coverage: (1) the Initial Deductible (in some plans), (2) the Initial Coverage phase, and (4) Catastrophic Coverage (where you have a $0 copay for formulary drugs).
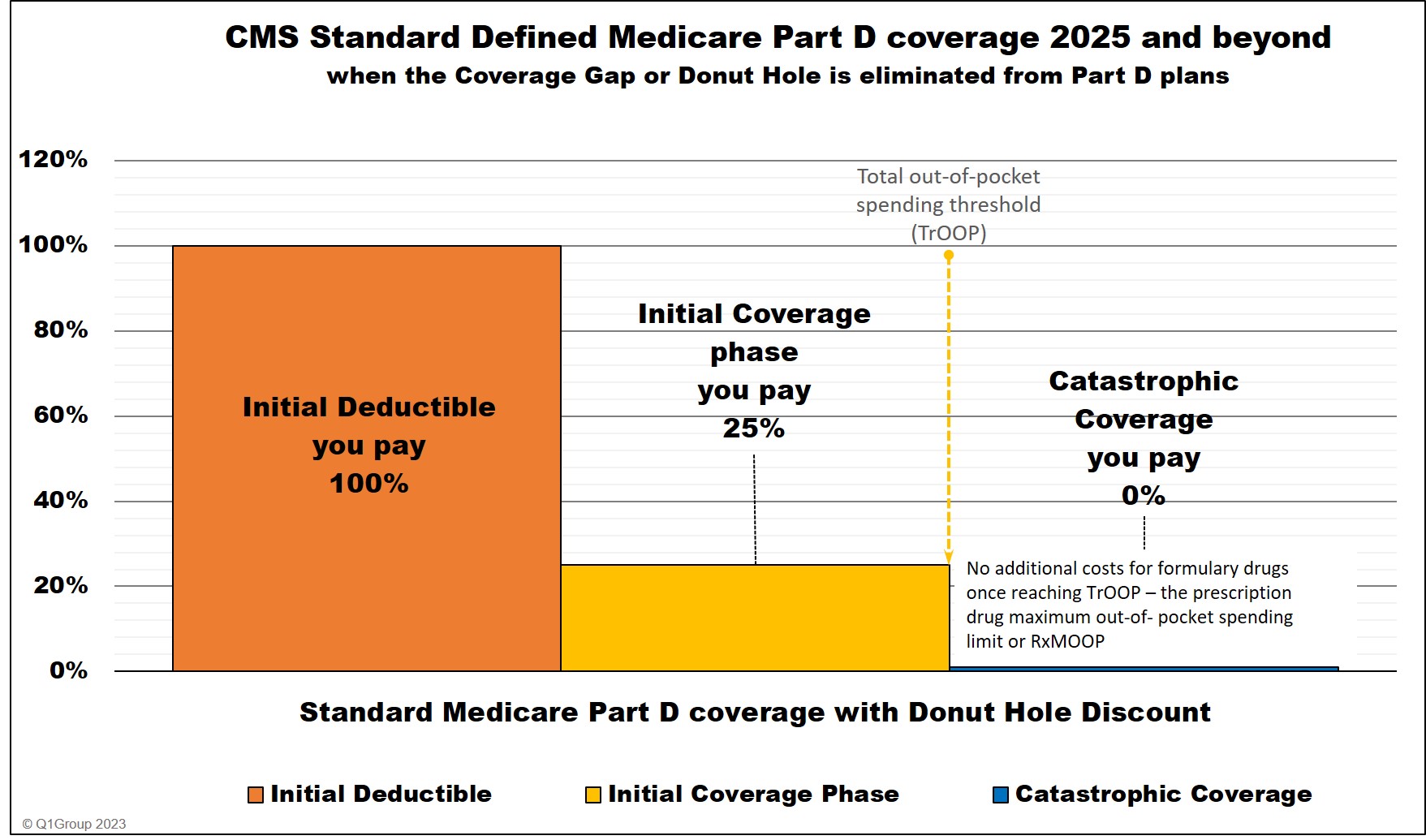
You move through these stages of your Medicare drug coverage either based on the amount of money you spend on formulary drugs (and in some cases what others pay on your behalf). Most people remain in the Initial Coverage phase for the year with only a small percentage of Medicare beneficiaries ever entering the Catastrophic Coverage phase.
(1) The Initial Deductible is where you pay 100% of your retail drug costs until you reach your deductible amount ($590 in 2025 and $615 in 2026). Many people enroll in a Medicare prescription drug plan with a $0 deductible and effectively skip-over this first phase.
(2) The Initial Coverage phase is the part of your drug coverage where you and your Medicare Part D plan share the cost of your formulary medications either as a fixed copay or a percentage of retail cost. Standard cost-sharing in the Initial Coverage phase is 25%, but your Medicare drug plan may have fixed copays for different formulary tiers. For example, if you purchase a mediation with a $100 retail cost, you may pay a $30 copay (and the plan pays $70) or you pay $25 coinsurance (and the plan pays $75). And since most people remain in their Medicare Part D plan's Initial Coverage phase, most people will consistently pay about the same price for their formulary drugs (or relatively the same price as retail drug prices increase) throughout the whole year.
(3) The Catastrophic Coverage phase is the last phase of your Medicare Part D plan and you enter once your total out-of-pocket drug costs (TrOOP) exceed a certain point ($2,000 in 2025 and $2,100 in 2026). Once you enter the Catastrophic Coverage phase, you will have no cost ($0) for all formulary medications for the remainder of the year.
As a review, 2025 Medicare Part D prescription drug plans have three different parts of coverage: (1) the Initial Deductible (in some plans), (2) the Initial Coverage phase, and (4) Catastrophic Coverage (where you have a $0 copay for formulary drugs).
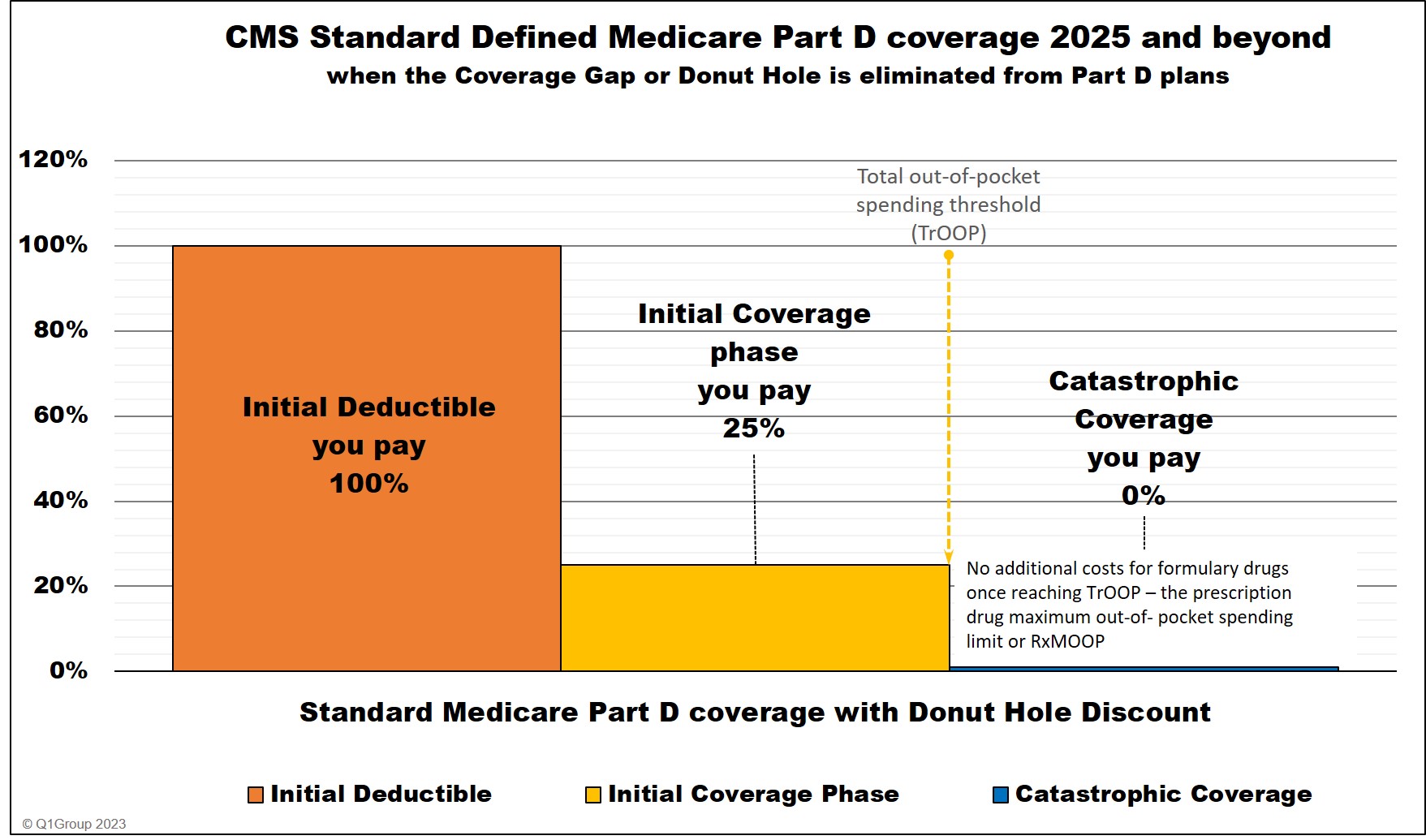
You move through these stages of your Medicare drug coverage either based on the amount of money you spend on formulary drugs (and in some cases what others pay on your behalf). Most people remain in the Initial Coverage phase for the year with only a small percentage of Medicare beneficiaries ever entering the Catastrophic Coverage phase.
(1) The Initial Deductible is where you pay 100% of your retail drug costs until you reach your deductible amount ($590 in 2025 and $615 in 2026). Many people enroll in a Medicare prescription drug plan with a $0 deductible and effectively skip-over this first phase.
(2) The Initial Coverage phase is the part of your drug coverage where you and your Medicare Part D plan share the cost of your formulary medications either as a fixed copay or a percentage of retail cost. Standard cost-sharing in the Initial Coverage phase is 25%, but your Medicare drug plan may have fixed copays for different formulary tiers. For example, if you purchase a mediation with a $100 retail cost, you may pay a $30 copay (and the plan pays $70) or you pay $25 coinsurance (and the plan pays $75). And since most people remain in their Medicare Part D plan's Initial Coverage phase, most people will consistently pay about the same price for their formulary drugs (or relatively the same price as retail drug prices increase) throughout the whole year.
(3) The Catastrophic Coverage phase is the last phase of your Medicare Part D plan and you enter once your total out-of-pocket drug costs (TrOOP) exceed a certain point ($2,000 in 2025 and $2,100 in 2026). Once you enter the Catastrophic Coverage phase, you will have no cost ($0) for all formulary medications for the remainder of the year.
Entering the Initial Coverage Phase
If your Medicare Part D plan has an Initial Deductible (the first phase of drug coverage), you will pay the Initial Deductible before entering the Initial Coverage phase.
However, some Medicare Part D plans have an Initial Deductible, but exclude the lower-costing (Tiers 1 and Tier 2) drugs from the deductible, so you skip the deductible for any of these low-costing formulary drugs and start in at your Initial Coverage phase for these drugs. In addition, all insulins covered by a Medicare drug plan are not be subject to the plan's deductible and are treated as if the purchase was in the Initial Coverage phase.
If your Medicare plan has a $0 deductible, you enter the Initial Coverage phase immediately, skipping over the first phase.
Exiting the Initial Coverage phase and entering the 2025 Catastrophic Coverage phase
When your out-of-pocket spending (TrOOP) reaches the out-of-pocket spending threshold (RxMOOP), you will leave your Initial Coverage phase and enter the Catastrophic Coverage phase where you will have no cost-sharing for all formulary drugs purchased through the remainder of the year.
A bit of history . . .
Prior to 2025, Medicare Part D coverage was different . . .
As a review, 2024 Medicare Part D prescription drug plans had four different parts of coverage: (1) the Initial Deductible (in some plans), (2) the Initial Coverage phase, (3) the Coverage Gap (Donut Hole), and (4) Catastrophic Coverage (where you will have a $0 copay for formulary drugs).
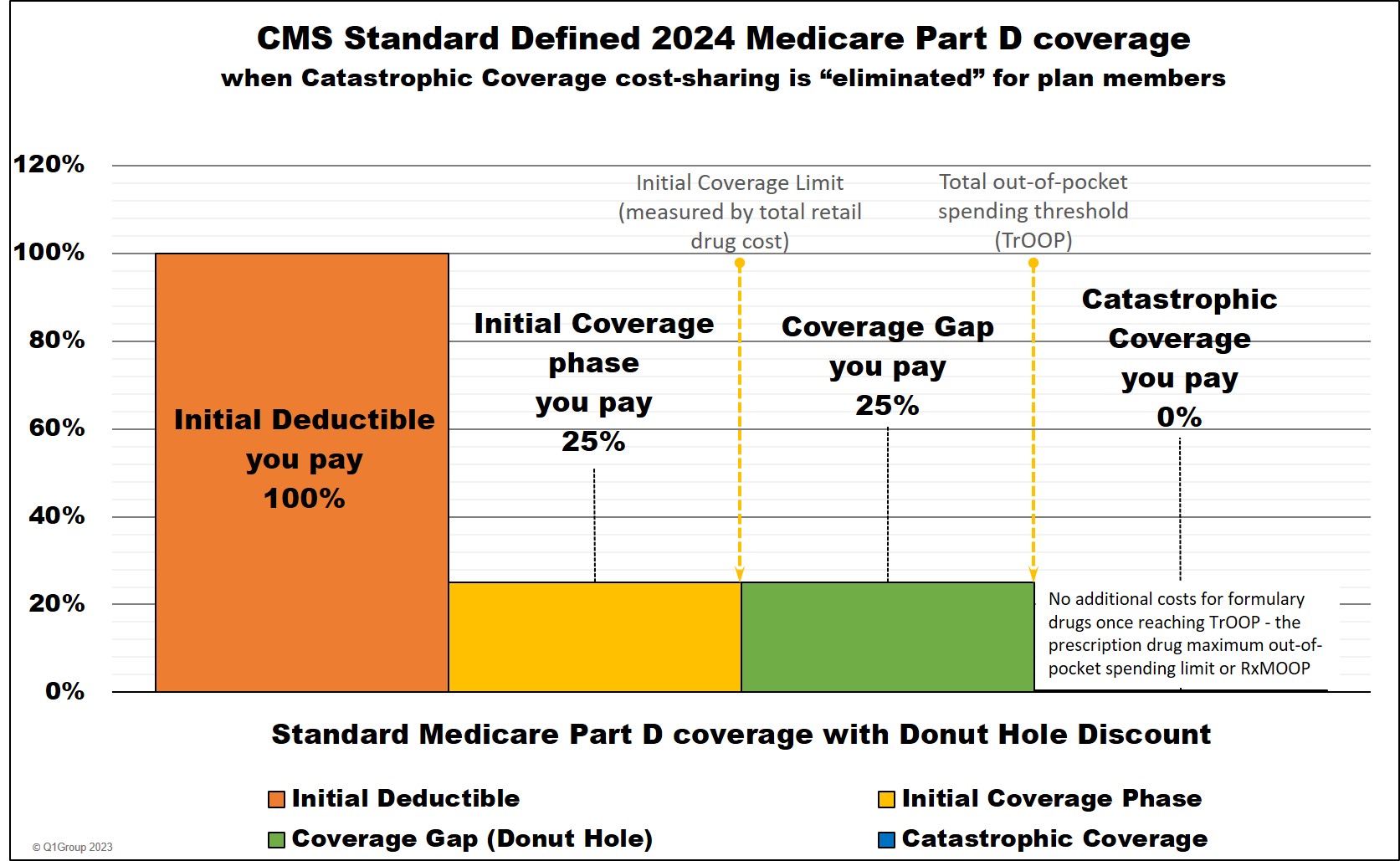
You moved through these stages of your Medicare drug coverage either based on the amount of money you spent on formulary drugs or the retail value of your prescription drug purchases, depending on the coverage phase. Most people remained in the Initial Coverage phase for the year with only a small percentage of Medicare beneficiaries ever entering the Coverage Gap or Catastrophic Coverage phase.
(1) The Initial Deductible phase was and remains where you pay 100% of your retail drug costs until you reach your deductible amount ($545 in 2024 ). Many people were enrolled in a Medicare prescription drug plan with a $0 deductible and effectively skip-over this first phase.
(2) The Initial Coverage phase was and remains the part of your drug coverage where you and your Medicare Part D plan shared the cost of your formulary medications either as a fixed co-pay or a percentage of retail cost. Standard cost-sharing in the Initial Coverage phase is 25%, but your Medicare drug plan may have had fixed copays for different formulary tiers. For example, if you purchased a mediation with a $100 retail cost, you may have paid a $30 copay (and the plan pays $70) or you have paid $25 coinsurance (and the plan pays $75). And since most people remained in their Medicare Part D plan's Initial Coverage phase, most people consistently paid about the same price for their formulary drugs (or relatively the same price as retail drug prices increase) throughout the whole year.
(3) The Coverage Gap or Donut Hole was the plan phase you entered once you exceeded the Initial Coverage Limit and where you received the Donut Hole discount on any formulary drug purchases.
Important Fact: The Coverage Gap or Donut Hole was eliminated in 2025.
The Inflation Reduction Act (IRA) removed the Coverage Gap (Donut Hole) in 2025. Medicare Part D beneficiaries now stay in the Initial Coverage phase until they reach the maximum cap on out-of-pocket spending for Part D formulary drugs - RxMOOP - which is set at $2,000 for 2025. After reaching RxMOOP Medicare Part D beneficiaries have a $0 copay for all formulary drugs.
(4) The Catastrophic Coverage phase was and remains the last phase of your Medicare Part D plan and you enter once your total out-of-pocket drug costs (TrOOP) exceed a certain point (over $8,000 in 2024 and $2,000 in 2025). Once you enter the Catastrophic Coverage phase, you have no cost ($0) for all formulary medications for the remainder of the year.
Prior to 2025, Medicare Part D coverage was different . . .
As a review, 2024 Medicare Part D prescription drug plans had four different parts of coverage: (1) the Initial Deductible (in some plans), (2) the Initial Coverage phase, (3) the Coverage Gap (Donut Hole), and (4) Catastrophic Coverage (where you will have a $0 copay for formulary drugs).
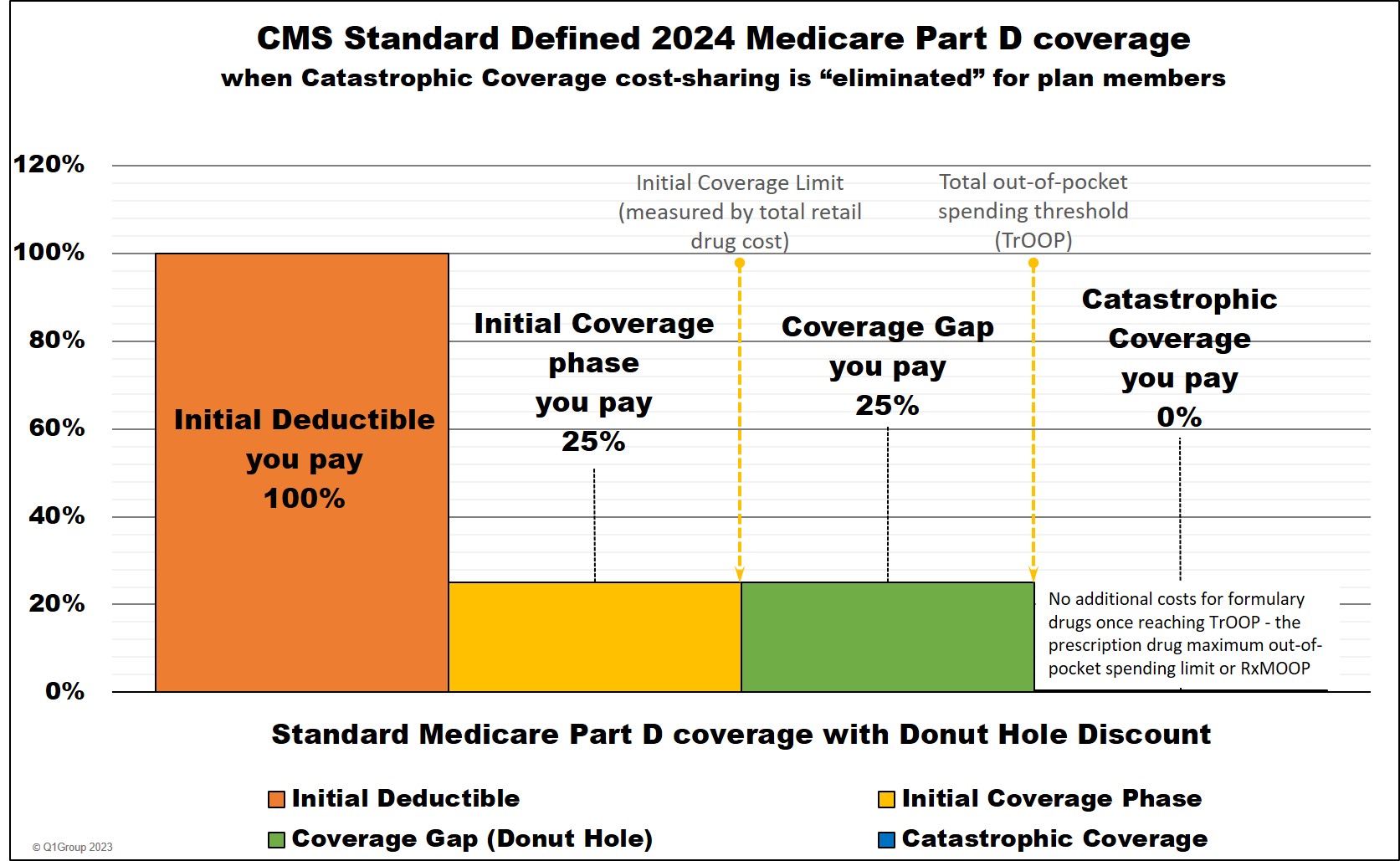
You moved through these stages of your Medicare drug coverage either based on the amount of money you spent on formulary drugs or the retail value of your prescription drug purchases, depending on the coverage phase. Most people remained in the Initial Coverage phase for the year with only a small percentage of Medicare beneficiaries ever entering the Coverage Gap or Catastrophic Coverage phase.
(1) The Initial Deductible phase was and remains where you pay 100% of your retail drug costs until you reach your deductible amount ($545 in 2024 ). Many people were enrolled in a Medicare prescription drug plan with a $0 deductible and effectively skip-over this first phase.
(2) The Initial Coverage phase was and remains the part of your drug coverage where you and your Medicare Part D plan shared the cost of your formulary medications either as a fixed co-pay or a percentage of retail cost. Standard cost-sharing in the Initial Coverage phase is 25%, but your Medicare drug plan may have had fixed copays for different formulary tiers. For example, if you purchased a mediation with a $100 retail cost, you may have paid a $30 copay (and the plan pays $70) or you have paid $25 coinsurance (and the plan pays $75). And since most people remained in their Medicare Part D plan's Initial Coverage phase, most people consistently paid about the same price for their formulary drugs (or relatively the same price as retail drug prices increase) throughout the whole year.
(3) The Coverage Gap or Donut Hole was the plan phase you entered once you exceeded the Initial Coverage Limit and where you received the Donut Hole discount on any formulary drug purchases.
Important Fact: The Coverage Gap or Donut Hole was eliminated in 2025.
The Inflation Reduction Act (IRA) removed the Coverage Gap (Donut Hole) in 2025. Medicare Part D beneficiaries now stay in the Initial Coverage phase until they reach the maximum cap on out-of-pocket spending for Part D formulary drugs - RxMOOP - which is set at $2,000 for 2025. After reaching RxMOOP Medicare Part D beneficiaries have a $0 copay for all formulary drugs.
(4) The Catastrophic Coverage phase was and remains the last phase of your Medicare Part D plan and you enter once your total out-of-pocket drug costs (TrOOP) exceed a certain point (over $8,000 in 2024 and $2,000 in 2025). Once you enter the Catastrophic Coverage phase, you have no cost ($0) for all formulary medications for the remainder of the year.
Browse FAQ Categories
Pets are Family Too!
Use your drug discount card to save on medications for the entire family ‐ including your pets.
- No enrollment fee and no limits on usage
- Everyone in your household can use the same card, including your pets
Your drug discount card is available to you at no cost.
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2025 Medicare Part D plan Facts & Figures
- 2025 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2024/2025 Medicare Part D plan changes
- 2025 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2024 to 2025
- Drug Finder: 2025 Medicare Part D drug search
- Formulary Browser: View any 2025 Medicare plan's drug list
- 2025 Browse Drugs By Letter
- Guide to Consumer Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2026 Medicare Part D Reminder Service
