What are the Medicare Part D Basic and Supplemental premiums?
Your monthly Medicare Part D premium can be broken into two parts: the Basic and Supplemental premiums - and Medicare provides the technical definitions of Total Premium, Basic Premium, and Supplemental Premium:
2024 Update: Starting in plan year 2024, partial LIS benefits were eliminated and the full LIS benefits were extended to include those persons who previously only qualified for partial benefits.
The Basic and Supplemental Medicare Part D Premium and Medicare Part D Extra Help
A person who qualifies for Extra Help benefits will pay either no Medicare plan premium ($0 depending on the plan) or pay only a portion of the “full premium”.
The LIS benchmark premiums are released every year and establish the maximum premium subsidy that would completely pay the monthly Medicare Part D premiums for people who qualify to receive LIS benefits. The LIS $0 benchmark premium is usually slightly different for every CMS Part D region.

If you qualify for the Medicare Part D Low-Income Subsidy and enroll in a "basic" (DS, AE, or BA) Medicare Part D plan with a monthly premium at or below your state’s LIS premium benchmark, you should have a $0 monthly premium for your Part D drug coverage. If you qualify for LIS benefits, but choose a Part D plan with a premium higher than the state benchmark, you may pay a portion of your premium that exceeds your state’s benchmark.
For example, the 2024 California $0 LIS Benchmark Premium is $40.98 and if you qualify for Extra Help and enrolled in a "basic" Medicare Part D plan with a premium below (or slightly over) the benchmark, you would pay a $0 premium. So if you chose the 2024 Wellcare Classic (PDP) Medicare Part D plan that has a $35.90 premium, you would pay a $0 premium.

You can see more about a state’s benchmark premium in our article:
"2025 State Low-Income Subsidy Benchmark Premium Amounts - with a comparison of benchmark changes since 2006"
here: Q1News.com/443.
Example: Your Medicare Part D premium when you are qualified for LIS or Extra Help
If you qualify for the LIS subsidy, and you have chosen to enroll into a Medicare Part D prescription drug plan that does not qualify for your state's Low-Income Subsidy $0 monthly premium, then you are responsible for a portion of your monthly premium that is above the state's benchmark premium.
For example, if you enrolled in the 2024 AARP MedicareRx Saver Plus (PDP) that has a $89.80 premium, you would pay $48.80 per month premium (roughly the $89.80 premium - the $40.98 benchmark premium).

Still another example . . .
Using California as our 2024 example state that has a $40.98 benchmark premium, and assuming you qualify for Extra Help benefits and decide to join the 2024 Wellcare Value Script (PDP) that has a $0.40 monthly premium, you would pay a monthly premium of $0.40 because the plan has "enhanced" features with a $18.10 Supplemental premium - and a ($-17.70) Basic premium - and, in short, does not qualify for the $0 premium even though the $0.40 premium is well below the state's $40.98 benchmark premium.

See also our question:
What are the Medicare Part D abbreviations: EA BA DS AE in the plan benefit type?
“Part D Total Premium: The Part D Total Premium is the sum of the Basic and Supplemental Premiums. Note the [Medicare] Part D Total Premium is net of any Part A/B rebates applied to "buy down" the drug premium for Medicare Advantage plans; for some plans the total premium may be lower than the sum of the basic and supplemental premiums due to negative basic or supplemental premiums.Although only the “total premium” is important to most people considering a Medicare Advantage plan (MAPD) or Medicare Part D plan (PDP), we also provide the Part D Basic Premium and Supplemental Premium information within our Medicare Part D Plan Finder (PDP-Finder.com) and Medicare Advantage Plan Finder (MA-Finder.com) since this information can be used by Medicare beneficiaries to understand how much they will pay per month for a Medicare Part D plan if they are eligible for the Low-Income Subsidy (LIS).
Part D Basic Premium: The Part D Basic Premium covers the basic prescription benefit only and does not cover enhanced drug benefits, medical benefits, or hospital benefits. Note: the Part D Basic Premium is net of any Part A/B rebates applied to "buy down" the drug premium for Medicare Advantage plans. Beneficiaries are also responsible for their Part B premium and any premiums for Medigap coverage to meet their individual needs.
Part D Supplemental Premium: The Part D Supplemental Premium covers any enhanced benefits that may be offered by a plan above and beyond the basic (standard) Part D benefit. These benefits may include extra coverage in the coverage gap, lower copayments than the standard benefit, coverage of non-Part D drugs. Note: the Part D Supplemental Premium is net of any Part A/B rebates applied to "buy down" the drug premium for Medicare Advantage plans.”
2024 Update: Starting in plan year 2024, partial LIS benefits were eliminated and the full LIS benefits were extended to include those persons who previously only qualified for partial benefits.
The Basic and Supplemental Medicare Part D Premium and Medicare Part D Extra Help
A person who qualifies for Extra Help benefits will pay either no Medicare plan premium ($0 depending on the plan) or pay only a portion of the “full premium”.
There are two situation when a Extra Help beneficiary may pay a partial premium.
(1) If the plan has a supplemental Part D premium, and
(2) If the plan's basic Part D premium is more than their state's Benchmark $0 LIS premium.
The LIS benchmark premiums are released every year and establish the maximum premium subsidy that would completely pay the monthly Medicare Part D premiums for people who qualify to receive LIS benefits. The LIS $0 benchmark premium is usually slightly different for every CMS Part D region.

If you qualify for the Medicare Part D Low-Income Subsidy and enroll in a "basic" (DS, AE, or BA) Medicare Part D plan with a monthly premium at or below your state’s LIS premium benchmark, you should have a $0 monthly premium for your Part D drug coverage. If you qualify for LIS benefits, but choose a Part D plan with a premium higher than the state benchmark, you may pay a portion of your premium that exceeds your state’s benchmark.
For example, the 2024 California $0 LIS Benchmark Premium is $40.98 and if you qualify for Extra Help and enrolled in a "basic" Medicare Part D plan with a premium below (or slightly over) the benchmark, you would pay a $0 premium. So if you chose the 2024 Wellcare Classic (PDP) Medicare Part D plan that has a $35.90 premium, you would pay a $0 premium.

You can see more about a state’s benchmark premium in our article:
"2025 State Low-Income Subsidy Benchmark Premium Amounts - with a comparison of benchmark changes since 2006"
here: Q1News.com/443.
Example: Your Medicare Part D premium when you are qualified for LIS or Extra Help
If you qualify for the LIS subsidy, and you have chosen to enroll into a Medicare Part D prescription drug plan that does not qualify for your state's Low-Income Subsidy $0 monthly premium, then you are responsible for a portion of your monthly premium that is above the state's benchmark premium.
For example, if you enrolled in the 2024 AARP MedicareRx Saver Plus (PDP) that has a $89.80 premium, you would pay $48.80 per month premium (roughly the $89.80 premium - the $40.98 benchmark premium).

Still another example . . .
Using California as our 2024 example state that has a $40.98 benchmark premium, and assuming you qualify for Extra Help benefits and decide to join the 2024 Wellcare Value Script (PDP) that has a $0.40 monthly premium, you would pay a monthly premium of $0.40 because the plan has "enhanced" features with a $18.10 Supplemental premium - and a ($-17.70) Basic premium - and, in short, does not qualify for the $0 premium even though the $0.40 premium is well below the state's $40.98 benchmark premium.

See also our question:
What are the Medicare Part D abbreviations: EA BA DS AE in the plan benefit type?
Pre-2024 - A bit of Medicare Part D history... Premiums dependent on Full or Partial-LIS Benefits
Prior to plan year 2024, Medicare beneficiaries may have only received partial-LIS. The Inflation Reduction Act (IRA) expanded the Extra Help program to provide full-LIS benefits to people who formerly only received partial-LIS.
Older 2023 example: Your 2023 Medicare Part D premium when you are qualified for less than 100% LIS
If you no longer qualify for full Extra Help Benefits (less than 100%), you may pay a higher portion of your Medicare Part D plan's premium - even when the Medicare Part D prescription drug plan qualifies for the $0 monthly Low-Income Subsidy premium.
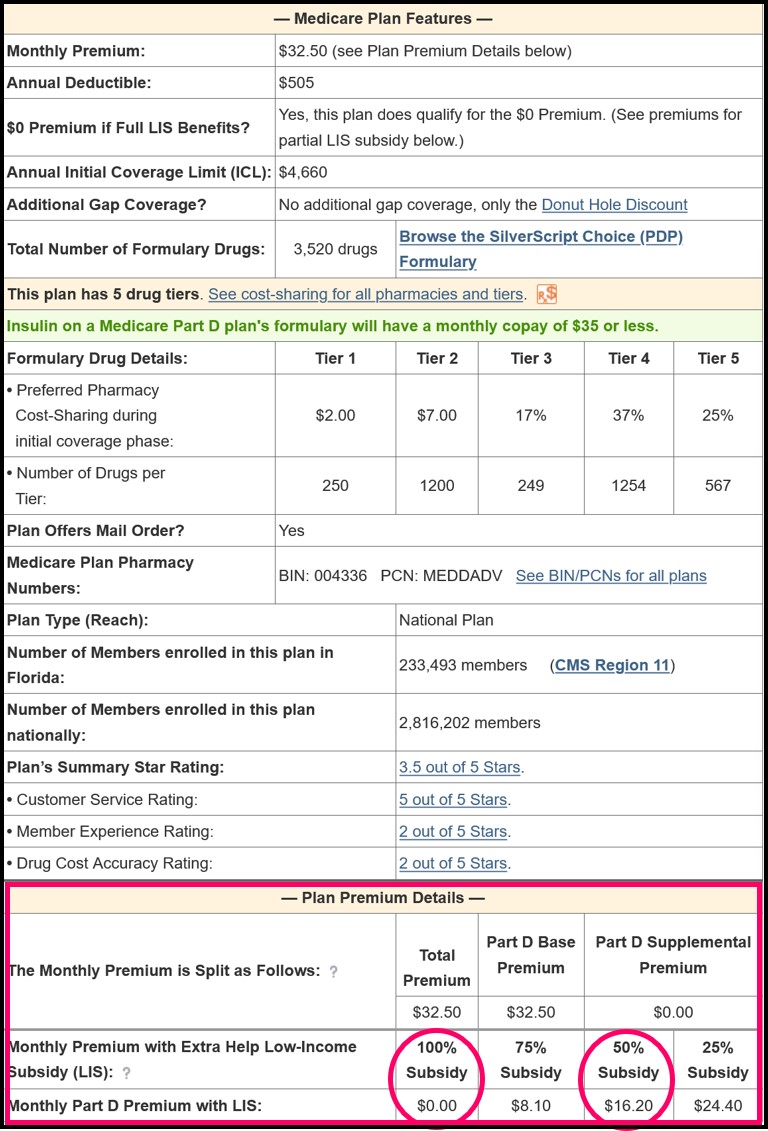
Using the same above example of the Florida 2023 SilverScript Choice (PDP) Medicare Part D plan that had a $32.50 premium, you would pay a $0 premium with full (100%) Extra Help benefits.
But, if you were eligible for only partial Extra Help benefits, you would pay a higher premium (although still less than the full $32.50 premium). In our example, if you qualified for 50% Extra Help, you would pay a premium of $16.20.
2023 Example: Paying the premium balance when you are qualified for full Extra Help, but you have chosen a Medicare Part D plan with a premium well above the state benchmark premium.
In this example, if you qualify for full Extra Help benefits, and your state has a LIS $0 premium benchmark of $35.92, - and you wish to join a Medicare Part D plan with a premium of $83.40 – you will not pay the full $83.40 premium with your LIS status, but instead, you will pay only a portion of the total premium.
In this example, of the $83.40 total premium, $64.80 is the basic premium and this basic premium is over the state’s $35.92 benchmark premium . . .
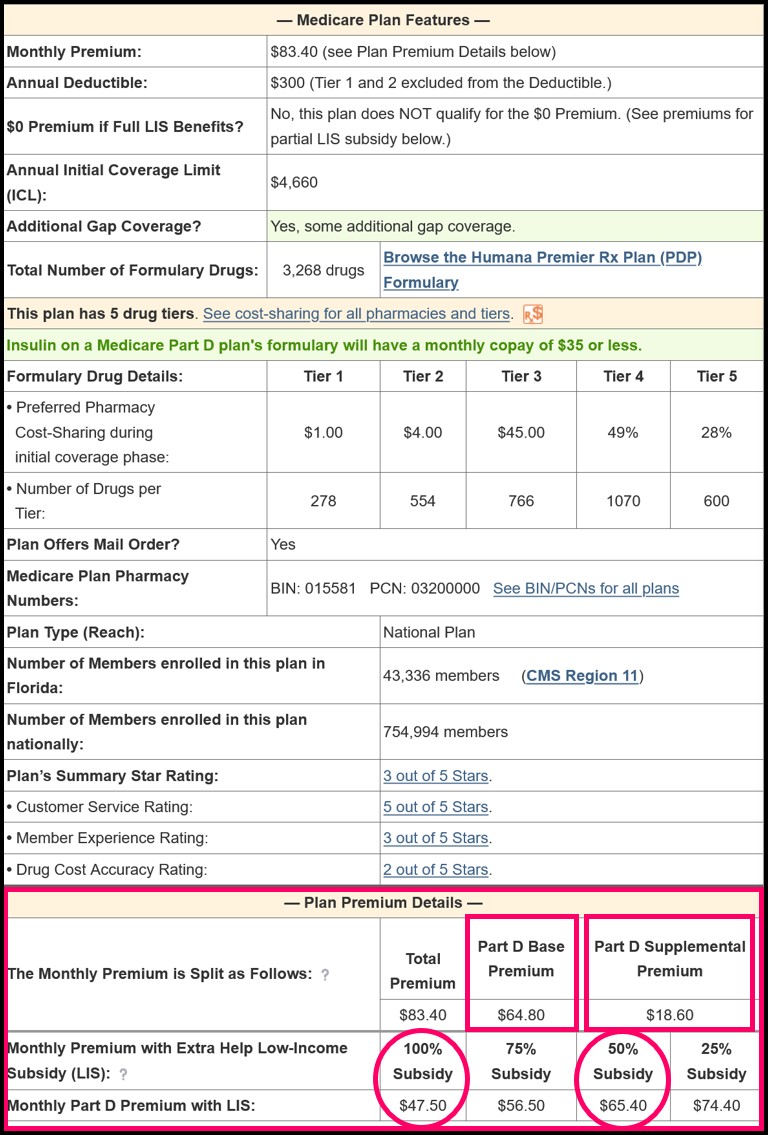
So if you receive 100% Extra Help (or are dual Medicare/Medicaid eligible), you will pay the portion of the Basic Premium over the benchmark plus the Supplemental premium. That is, the amount of the basic premium that is not covered by the state benchmark premium + the supplemental premium, in this example $47.50, as shown in the graphic.
$64.80 Basic Premium - $35.92 Benchmark Premium
+ $18.60 Supplemental Premium
------------------------------------------------------------------
= $47.48 (rounded to $47.50)
Browse FAQ Categories
Pets are Family Too!
Use your drug discount card to save on medications for the entire family ‐ including your pets.
- No enrollment fee and no limits on usage
- Everyone in your household can use the same card, including your pets
Your drug discount card is available to you at no cost.
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2025 Medicare Part D plan Facts & Figures
- 2025 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2024/2025 Medicare Part D plan changes
- 2025 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2024 to 2025
- Drug Finder: 2025 Medicare Part D drug search
- Formulary Browser: View any 2025 Medicare plan's drug list
- 2025 Browse Drugs By Letter
- Guide to Consumer Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2026 Medicare Part D Reminder Service
