What will I pay when my Medicare Part D drug plan excludes Tier 1 and Tier 2 drugs from the plan's initial deductible?
You will only pay the Tier 1 or Tier 2 copayment for your medications if Tier 1 and Tier 2 formulary drugs are excluded from your Medicare Part D plan's initial deductible - even when your plan's initial deductible is not yet met.
Question: Do many 2025 Medicare Part D plans exclude some formulary medications from the deductible?
Over 37% of all stand-alone 2025 Medicare Part D drug plans exclude some formulary tiers from the plan's deductible. Although 85% of all stand-alone 2025 Medicare Part D prescription drug plans have an initial deductible, about 44% of all 2025 Part D drug plans with a deductible exclude some low-costing formulary tiers from the plan's deductible. Over the past years, we have seen an increasing number of Medicare Part D drug plans now exclude low-cost formulary Tier 1 and Tier 2 drugs from the plan's initial deductible, providing you with immediate coverage for many low-costing drugs. This means, from the very start of the plan year, you will pay just Tier 1 and 2 copays for these drugs (unless the retail price is less than the copay and then you will pay no more than the retail price) - and your initial deductible will only be applied to more-expensive brand-name drugs or drugs on higher formulary tiers that are not excluded from the deductible.
Question: So what happens when my plan does not exclude formulary drugs from the deductible?
You pay the full retail drug price until you meet your deductible. If your Medicare Part D plan does not exclude any tiers from the initial deductible, then you must pay your Medicare Part D plan's initial deductible before you receive any coverage from your Medicare Part D plan. For example, the standard 2025 Medicare Part D deductible is $590 (increasing to $615 in 2026) and you must pay the full retail price for your formulary drugs until you have spent $590 out of pocket. When the initial deductible is met, then the Medicare plan coverage begins and you will only pay a portion of the retail drug cost, sharing the retail drug cost with your Medicare drug plan (and the pharmaceutical manufacturer and the United States government).
Example Purchase #1: What will I pay when my first purchase of the year is a $22 Tier 2 drug excluded from my deductible?
You will pay your plan’s $3 Tier 2 copay. Your purchase of low-costing Tier 2 drugs drugs are not impacted by your plan's initial deductible and you have immediate coverage of Tier 1 and Tier 2 formulary drugs as if you were in your plan's Initial Coverage Phase.
Example Purchase #2: Up to this point in the year, you have only purchased Tier 1 and Tier 2 drugs that are excluded from the Initial Deductible and you now have a newly-prescribed Tier 3 drug with a retail cost of $520 and a $47 Tier 3 copay.
You will pay your the full $520 retail drug price for the Tier 3 drug.
Example Purchase #3: Up to this point in the year, you have only purchased Tier 1 and Tier 2 drugs that are excluded from the Initial Deductible and you now have a newly-prescribed Tier 3 drug with a retail cost of $610 and a $47 Tier 3 copay.
(Note: this a straddle claim).
You will pay a total of $610 (the full retail drug price) for the $610 Tier 3 drug.
(1) Initial Deductible: You would first pay $590 of the $610 retail drug cost to satisfy your $590 Initial Deductible and
(2) Initial Coverage Phase: the remaining $20 portion of the retail cost ($610 - $590) would carry over (straddle) into your Initial Coverage phase where you have a $47 copay. But, since you never pay more than the drug plan’s retail cost, you are not charged the full $47 copay, but instead, you pay the remaining $20 retail balance, so your total cost-sharing would be $610 ($590 + $20).
Question: But what happens if I only buy Tier 1 and Tier 2 formulary drugs excluded from the plan's deductible, will I ever enter Catastrophic Coverage by reaching the annual $2,000 out-of-pocket spending limit?
Yes. In the examples above (with Tier 1 and Tier 2 drugs excluded from the deductible), if you were to only purchase Tier 1 and Tier 2 drugs all year, your $590 initial deductible would never be met. However, you enter Catastrophic Coverage when what you spend (or other people spend on your behalf) on formulary Part D drugs reaches the $2,000 maximum out-of-pocket spending limit or RxMOOP.
A note on Medicare Part D coverage prior to 2025:
Question: Do many 2025 Medicare Part D plans exclude some formulary medications from the deductible?
Over 37% of all stand-alone 2025 Medicare Part D drug plans exclude some formulary tiers from the plan's deductible. Although 85% of all stand-alone 2025 Medicare Part D prescription drug plans have an initial deductible, about 44% of all 2025 Part D drug plans with a deductible exclude some low-costing formulary tiers from the plan's deductible. Over the past years, we have seen an increasing number of Medicare Part D drug plans now exclude low-cost formulary Tier 1 and Tier 2 drugs from the plan's initial deductible, providing you with immediate coverage for many low-costing drugs. This means, from the very start of the plan year, you will pay just Tier 1 and 2 copays for these drugs (unless the retail price is less than the copay and then you will pay no more than the retail price) - and your initial deductible will only be applied to more-expensive brand-name drugs or drugs on higher formulary tiers that are not excluded from the deductible.
Question: So what happens when my plan does not exclude formulary drugs from the deductible?
You pay the full retail drug price until you meet your deductible. If your Medicare Part D plan does not exclude any tiers from the initial deductible, then you must pay your Medicare Part D plan's initial deductible before you receive any coverage from your Medicare Part D plan. For example, the standard 2025 Medicare Part D deductible is $590 (increasing to $615 in 2026) and you must pay the full retail price for your formulary drugs until you have spent $590 out of pocket. When the initial deductible is met, then the Medicare plan coverage begins and you will only pay a portion of the retail drug cost, sharing the retail drug cost with your Medicare drug plan (and the pharmaceutical manufacturer and the United States government).
Example Purchase #1: What will I pay when my first purchase of the year is a $22 Tier 2 drug excluded from my deductible?
You will pay your plan’s $3 Tier 2 copay. Your purchase of low-costing Tier 2 drugs drugs are not impacted by your plan's initial deductible and you have immediate coverage of Tier 1 and Tier 2 formulary drugs as if you were in your plan's Initial Coverage Phase.
- Your Medicare Part D plan's initial deductible: $590 (still unchanged)
- Your plan's Tier 2 drug copay: $3
- Your Tier 2 drug's retail price: $22
- After the Tier 2 drug purchase your Medicare Part D plan's initial deductible: $590
Example Purchase #2: Up to this point in the year, you have only purchased Tier 1 and Tier 2 drugs that are excluded from the Initial Deductible and you now have a newly-prescribed Tier 3 drug with a retail cost of $520 and a $47 Tier 3 copay.
You will pay your the full $520 retail drug price for the Tier 3 drug.
- Your Medicare Part D plan's initial deductible was: $590 (still unchanged)
- Your plan's Tier 3 drug copay: $47
- Your Tier 3 drug's retail price: $520
-
After the Tier 3 drug purchase your Medicare Part D plan's initial deductible: $70 ($590 - $520)
Example Purchase #3: Up to this point in the year, you have only purchased Tier 1 and Tier 2 drugs that are excluded from the Initial Deductible and you now have a newly-prescribed Tier 3 drug with a retail cost of $610 and a $47 Tier 3 copay.
(Note: this a straddle claim).
You will pay a total of $610 (the full retail drug price) for the $610 Tier 3 drug.
- Your Medicare Part D plan's initial deductible was: $590 (still unchanged)
- Your plan's Tier 3 drug copay: $47
- Your Tier 3 drug's retail price: $610
- After the Tier 3 drug purchase your Medicare Part D plan's initial deductible: $0 (you are now in into Initial Coverage Phase)
(1) Initial Deductible: You would first pay $590 of the $610 retail drug cost to satisfy your $590 Initial Deductible and
(2) Initial Coverage Phase: the remaining $20 portion of the retail cost ($610 - $590) would carry over (straddle) into your Initial Coverage phase where you have a $47 copay. But, since you never pay more than the drug plan’s retail cost, you are not charged the full $47 copay, but instead, you pay the remaining $20 retail balance, so your total cost-sharing would be $610 ($590 + $20).
Question: But what happens if I only buy Tier 1 and Tier 2 formulary drugs excluded from the plan's deductible, will I ever enter Catastrophic Coverage by reaching the annual $2,000 out-of-pocket spending limit?
Yes. In the examples above (with Tier 1 and Tier 2 drugs excluded from the deductible), if you were to only purchase Tier 1 and Tier 2 drugs all year, your $590 initial deductible would never be met. However, you enter Catastrophic Coverage when what you spend (or other people spend on your behalf) on formulary Part D drugs reaches the $2,000 maximum out-of-pocket spending limit or RxMOOP.
A note on Medicare Part D coverage prior to 2025:
If your total 2024 retail drug cost
exceeded your Initial Coverage Limit ($5,030 in 2024), you would enter your plan's Coverage Gap or Donut Hole - and continue to move through your plan's coverage - and the plan's initial deductible is no longer an issue - even when you had not met your 2024 deductible of $545. As noted by Medicare in the September 10, 2010 memorandum, "Additional Guidance Concerning Closing the Coverage Gap in 2011",
"With the implementation of the [Medicare Coverage Gap Discount Program], however, CMS finds it necessary to clarify that for purposes of the [Medicare Coverage Gap Discount Program] only beginning in 2011, a Part D deductible ceases to apply once a beneficiary’s total gross covered drug costs exceed the [Initial Coverage Limit]. This means that for a beneficiary enrolled in a Part D plan with a brand-only deductible, applicable (i.e. brand) drugs that would otherwise be subject to the deductible will be eligible for a coverage gap discount once the beneficiary’s total gross covered drug costs exceed the [Initial Coverage Limit] even if the beneficiary has not satisfied the deductible."
Example Purchase #4: Up to this point you have only purchased Tier 1 and Tier 2 drugs that are excluded from the Initial Deductible and you now purchase a Tier 3 (or Tier 6) insulin drug with a retail cost of $300.
You will pay no more than $35 for any insulin product on your plan's formulary. You will pay a copay of no more than $35 for a 30-day supply of a formulary insulin product even though you have not met your plan's annual initial deductible.
- Your Medicare Part D plan's initial deductible: $590 (still unchanged)
- Your plan's Tier 3 insulin copay: $35
- Your Tier 3 or Tier 6 insulin retail price: $300
- After the Tier 3 drug purchase your Medicare Part D plan's initial deductible: $590
Historical note from 2023: Unlike a Tier excluded from the deductible (such as in the example above), the 2023 purchase of a plan's covered insulin product will reduce a person's initial deductible by the total retail cost of the insulin product - so not just the $35 or less copay paid by the person, but the retail price of the insulin.
For example, if a plan's negotiated retail cost for insulin was $200 and a person had not yet met the 2023 deductible of $505, the person will pay no more than $35 for the formulary insulin product, but the deductible will be reduced by the $200 retail insulin cost - and so the remaining 2023 deductible would now be $305.
- Your 2023 Medicare Part D plan's initial deductible: $505 (still unchanged)
- Your plan's Tier 3 insulin copay: $35
- Your Tier 3 insulin retail price: $300
- After the Tier 3 insulin purchase your 2023 Medicare Part D plan's initial deductible: $205
Historical note from 2024: As per Medicare guidance: "The [2024] deductible does not apply to the covered insulin product, therefore, none of the cost of the insulin product . . . would count towards satisfying the deductible that otherwise applies under the plan for other products." So an insulin purchase would be similar to the purchase of a Tier 1 or Tier 2 drug excluded from the deductible.
Question: How do you know whether a Medicare plan excludes Tier 1 and Tier 2 drugs from the initial deductible?
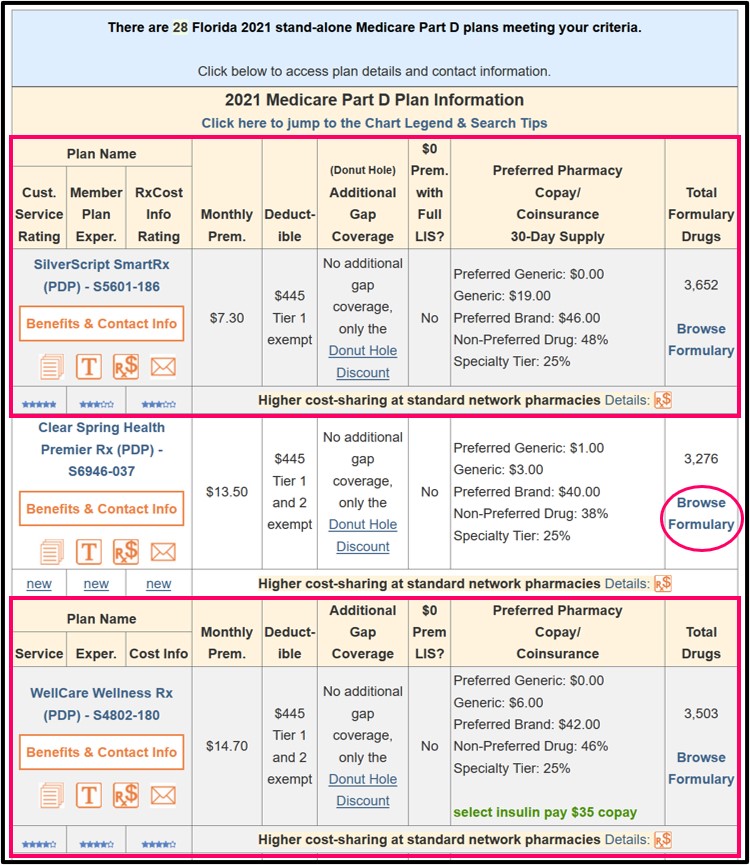
You will notice when you visit our Q1Medicare Medicare Part D Plan Finder (PDP-Finder.com) that Medicare Part D plans will be marked under the "Deductible" section with the text "Tier 1 exempt" or "Tier 1 and 2 exempt".
Here is an example of 2021 Florida Medicare Part D plans having lower-costing generics excluded from the standard deductible.
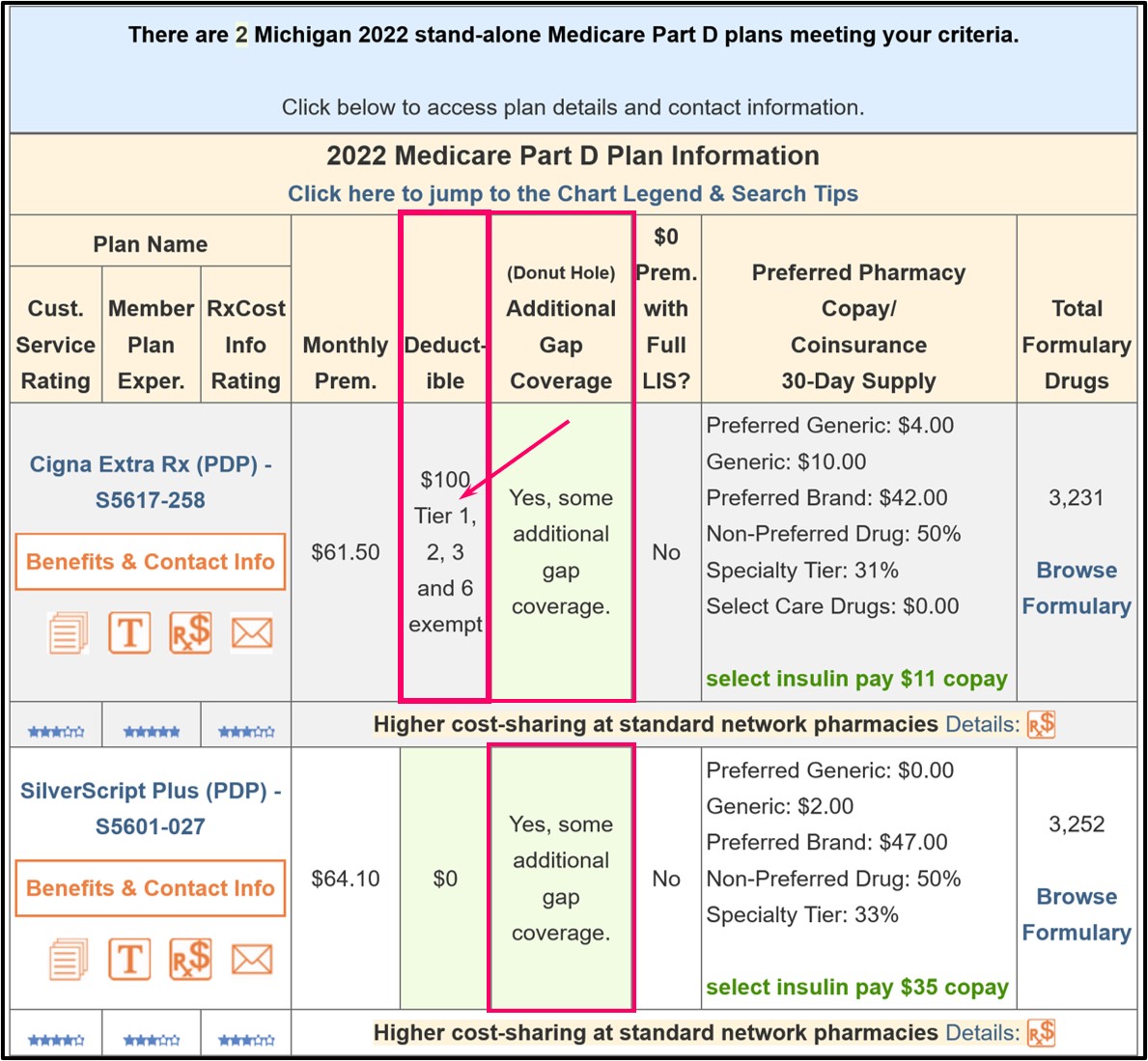
And here is an older example of a 2022 Medicare Part D plan having Tier 1, Tier 2, Tier 3, and Tier 6 drugs excluded from the plan's initial $100 deductible.
In addition, when you view the Medicare plan details (by clicking on the
Medicare plan name), you can see in the plan details that Tier 1 and
Tier 2 drugs may be excluded from the plan's initial deductible.
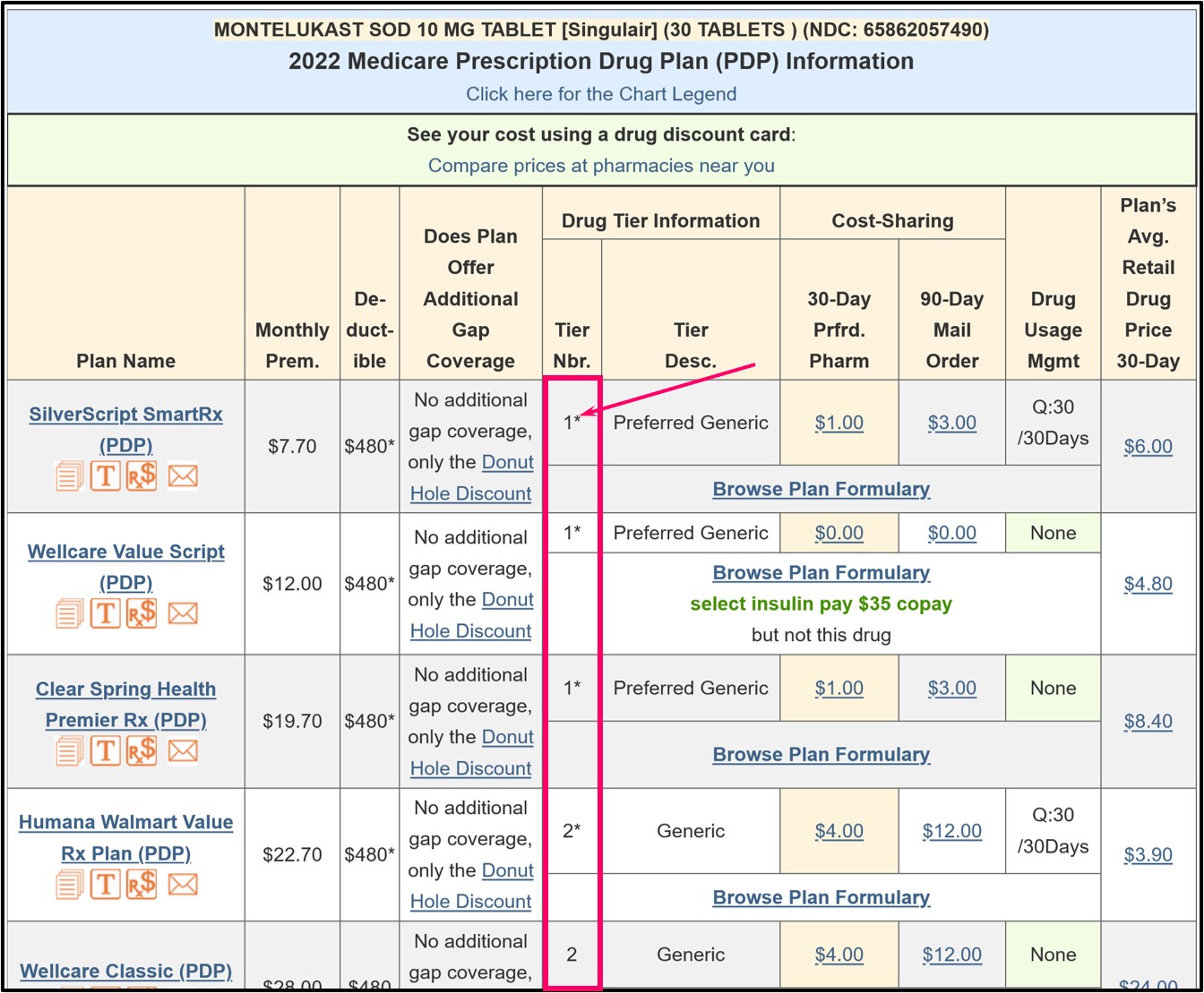
As an older example using the Q1Rx Drug Finder, in 2023, Florida has 23 stand-alone Medicare Part D plans that cover “MONTELUKAST SOD 10 MG TABLET [Singulair] (30 TABLETS) (NDC: 65862057490)” and you can click on the Medicare plan name to see more details of the coverage for a particular plan.
In the Q1Rx Drug Finder, you can see that some drugs are marked as (1* or 2*) and this means that the Tier 1 or Tier 2 drug has is excluded from the plan's initial deductible - and receives coverage according to the cost-sharing.
Need more help? -- Contact your Medicare plan and review your Medicare drug plan's documentation.
You can learn more by contacting your Medicare Part D prescription drug plan by calling the toll-free number for Member Services found on your Member ID card.
References include:
https://www.csscoperations.com/internet/Cssc.nsf/ files/PDEParticipantGuide%20cameraready%20081811.pdf/ $FIle/PDEParticipantGuide%20cameraready%20081811.pdf
https://www.hhs.gov/guidance/document/additional-guidance-concerning-closing-coverage-gap-2011
https://www.cms.gov/files/document/frequently-asked-questions-medicare-part-d-insulin-benefit.pdf
https://www.cms.gov/files/document/ira-2024-pdeguidance-final508g.pdf
As an older example using the Q1Rx Drug Finder, in 2023, Florida has 23 stand-alone Medicare Part D plans that cover “MONTELUKAST SOD 10 MG TABLET [Singulair] (30 TABLETS) (NDC: 65862057490)” and you can click on the Medicare plan name to see more details of the coverage for a particular plan.
In the Q1Rx Drug Finder, you can see that some drugs are marked as (1* or 2*) and this means that the Tier 1 or Tier 2 drug has is excluded from the plan's initial deductible - and receives coverage according to the cost-sharing.
Need more help? -- Contact your Medicare plan and review your Medicare drug plan's documentation.
You can learn more by contacting your Medicare Part D prescription drug plan by calling the toll-free number for Member Services found on your Member ID card.
Review your plan's Evidence of Coverage.
You can also read more about your drug plan coverage in your Medicare
plan's Evidence of Coverage document where you might find in Chapter 4,
"What you pay for your Part D prescription drugs":"During the Deductible Stage, you pay the full cost of your Cost-Sharing Tier 3, Cost-Sharing Tier 4, and Cost-Sharing Tier 5 drugs" and then, "You stay in the Deductible Stage until you have paid [annual deductible amount] for your Cost-Sharing Tier 3, Cost-Sharing Tier 4, and Cost-Sharing Tier 5 drugs".Further on in the Evidence of Coverage Chapter 4 you may read:
"The Deductible Stage is the first payment stage for your drug coverage. You will pay a yearly deductible of [annual deductible amount] on Cost-Sharing Tier 3, Cost-Sharing Tier 4, and Cost-Sharing Tier 5 drugs. You must pay the full cost of your Cost-Sharing Tier 3, Cost-Sharing Tier 4, and Cost-Sharing Tier 5 drugs until you reach the plan's deductible amount. For all other drugs you will not have to pay any deductible and will start receiving coverage immediately.
• Your "full cost" is usually lower than the normal full price of the drug, since our plan has negotiated lower costs for most drugs.
• The "deductible" is the amount you must pay for your Part D prescription drugs before the plan begins to pay its share.
Once you have paid [the annual deductible amount] for your Cost-Sharing Tier 3, Cost-Sharing Tier 4, and Cost-Sharing Tier 5 drugs, you leave the Deductible Stage and move on to the next drug payment stage, which is the Initial Coverage Stage."
References include:
https://www.csscoperations.com/internet/Cssc.nsf/ files/PDEParticipantGuide%20cameraready%20081811.pdf/ $FIle/PDEParticipantGuide%20cameraready%20081811.pdf
https://www.hhs.gov/guidance/document/additional-guidance-concerning-closing-coverage-gap-2011
https://www.cms.gov/files/document/frequently-asked-questions-medicare-part-d-insulin-benefit.pdf
https://www.cms.gov/files/document/ira-2024-pdeguidance-final508g.pdf
Browse FAQ Categories
Pets are Family Too!
Use your drug discount card to save on medications for the entire family ‐ including your pets.
- No enrollment fee and no limits on usage
- Everyone in your household can use the same card, including your pets
Your drug discount card is available to you at no cost.
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2025 Medicare Part D plan Facts & Figures
- 2025 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2024/2025 Medicare Part D plan changes
- 2025 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2024 to 2025
- Drug Finder: 2025 Medicare Part D drug search
- Formulary Browser: View any 2025 Medicare plan's drug list
- 2025 Browse Drugs By Letter
- Guide to Consumer Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2026 Medicare Part D Reminder Service