What is a Medicare Part D plan?
Medicare Part D prescription drug plans provide insurance coverage for your out-patient prescription drugs - and works just like any other type of insurance:
(1) Monthly premium. You usually pay a monthly premium for coverage from around $0 to $196 for 2024 stand-alone Prescription drug plans or $0 to $327 for a Medicare Advantage plan that has drug coverage.
(2) Deductible. You may pay an initial deductible where you are 100% responsible for your drug costs before you and your drug plan begin to share the cost of drug coverage (although some drug plans have a $0 deductible and some drug plans with a deductible exclude low-costing generics from the deductible), and
(3) Cost-Sharing. Once you are through your deductible (if any), you and your insurance share the cost of your formulary drugs. For example, you pay 25% of the retail drug price for your medication and your plan pays the remaining 75%, or you pay a flat $2 copay for your generic drugs that retail for $12 and your plan pays the balance.
(4) Limitations on coverage. A Medicare Part D plan (drug insurance) will not cover all medications and each Medicare drug plan can cover different drugs (or drug strengths). So, each year you need to carefully choose a drug plan with a formulary (drug list) that includes your prescriptions - with the knowledge that the formulary can change throughout the plan year (usually substituting newly-released generic drugs for higher-costing brand-name drugs).
(5) Annual drug plan changes. Every year your drug plan can (and usually will) change which drugs the plan covers and the cost associated with the covered drugs. For example, your drug plan may have covered the brand-name drug Lipitor® 10mg for $30, but next year no longer covers Lipitor and instead covers the generic equivalent, Atorvastatin 10mg for $3.
(6) Enrolling into a Medicare Part D drug plan. Just like other types of insurance, there are several ways to enroll into a Medicare drug plan. You can call a Medicare representative at 1-800-Medicare (1-800-633-4227). You can enroll directly though the Medicare plan by calling the plan's toll-free number (usually found on printed plan information or the plan's website. You can enroll through a local insurance agent that represents you chosen Medicare drug plan. You can use a website that represents several Medicare drug plans. For assistance with choosing a Medicare drug plan, you can also call or visit a volunteer such as a SHIP representative or someone at your local senior center.
Question: How do you get Medicare Part D prescription drug coverage?
Your Medicare Part D prescription drug coverage can be provided in several different ways:
No. Medicare Part D plans are not required to cover all other prescription drugs - but instead are only required to cover a fixed number of drugs in different therapeutic drug classes. The medications covered by a Medicare Part D plan are organized in a formulary or drug list and this list must cover at least two drugs in each drug category and all drugs (with a few exceptions) in the six therapeutic categories: antidepressants, antispychotics, anticonvulsants (drugs to preventseizures), antiretrovirals (drugs to treat HIV/AIDS), immunosuppressants, and antineoplastics (cancer drugs).
Question: How many different drugs does a Medicare Part D plan cover?
That depends on the drug plan. Each Medicare Part D plan will cover a different number of prescription drugs. In general, a Medicare Part D plan may include several thousand medications in different forms (for instance, 10mg, 20mg, and 40mg Advair Diskus MIS 250/50). Medicare Part D plans also cover vaccinations not covered by Medicare Part B (such as the Shingles Vaccine). Each year, a Medicare drug plan can change the plan's formulary. However, Medicare Part D Medicare Part D plans are regulated by the Centers for Medicare and Medicaid Services (CMS) and CMS must approve a Medicare plan's formulary or drug list every year.
Question: Are any medications excluded from every Medicare Part D plan?
Yes. Some prescription drugs are excluded from the Medicare Part D program by law (such as drugs for weight loss, erectile dysfunction, cosmetic purposes, or hair growth) - however, it is possible that your plan may provide supplemental coverage of these non-Part D drugs as "Bonus Drugs".
Tip: You can see all drugs covered by a particular Medicare plan by using our Q1Medicare Formulary Browser, you can change the name of the Medicare Part D plan and state to browse other formularies. You can also browse all Medicare Part D plans in a certain area that cover a specific medication - and at what cost using our Q1Medicare Drug Finder tool (found at Q1Rx.com).
Question: If I have employer drug coverage can I also join a Medicare Part D drug plan?
Probably not. Warning: If you have an employer health plan that includes prescription drug coverage - and then enroll in a Medicare Part D plan, you risk losing all of your employer health plan coverage, not just drug coverage. You can click here to read more in our Frequently Asked Questions about checking with your employer health plan administrator before enrolling in a Medicare prescription drug plan.
Question: If I have drug coverage through the Veterans Affairs (VA) can I join a Medicare Part D plan?
Yes. If you have VA coverage (that is, prescription drug coverage as part of Veterans Affairs benefits), then you may not need Medicare Part D coverage. However, if you find that the VA does not cover all of your medication needs, you can also enroll in a Medicare Part D program. The two programs cannot be used at the same time for the purchase of a single drug, but actually work together, allowing coordinated coverage - first under the VA and secondly under your Medicare Part D plan. Your VA coverage is also considered "creditable coverage" and should you decide to enroll in a Medicare Part D plan after the close of your initial enrollment period, there will be no penalty for late enrollment. You can click here to read more in our VA section of Frequently Asked Questions.
Question: Am I required to join a Medicare Part D plan?
No. The Medicare Part D program is voluntary and you are not required to enroll in a Medicare Part D plan when you first become eligible for Medicare. However, if you do not have some other form of creditable prescription drug coverage and later decide to join a Part D plan (PDP or MAPD) you may incur a permanent late-enrollment penalty that you will pay in addition to your monthly plan premiums.
Question: How do I enroll into a Medicare Part D plan?
As noted above, there are several ways to join a Part D plan and enrollment depends on your personal preference.
That depends on you. Choosing a Medicare plan may be somewhat based on your risk tolerance. For instance, people who are not taking any (or only a few generic) medications, can look up the lowest costing Medicare prescription drug plan (or Medicare Advantage plan that includes prescription coverage), check for medication coverage, and decide whether they want to:
People with more complex medication or healthcare needs must spend more time ensuring that their specific needs (medical and prescription drugs) are covered by a Medicare Part D or Medicare Advantage plan. For example, if you have a particular plan in mind (such as a local Medicare Advantage HMO POS that is provided by the large university or hospital system in your area), then you can review all of the coverage details we have online - and then call the plan to learn whether their healthcare providers are included in the Medicare Advantage plan's network.
Question: If I don't join a drug plan when I am first eligible, how is the Late-Enrollment Penalty calculated?
Late-Enrollment Penalties are assessed when you eligible for Medicare Part D coverage, but are without some form of creditable drug coverage for more than 63 days. You can click here to read more in our late-enrollment premium penalty section of Frequently Asked Questions. Late-enrollment penalties are permanent and can change (increase) year-to-year. You will pay 1% of the national base Medicare Part D premium $34.70 in 2024) for every month that you were without some creditable prescription drug coverage before you enrolled in a Medicare Part D plan. So if you were eligible for Medicare when you were 65 and now you are 70, you would pay a penalty based on 60 months without coverage (5 years * 12) or about 60% of the annual base premium (so around $34.70 * .6 = $20.80 per month in addition to your monthly Part D plan premium).
Question: Are all Medicare Part D plans about the same and available everywhere?
No. Medicare Part D coverage will vary plan-to-plan and not all Medicare plans are available in all areas of the country. Remember: Medicare Part D and Medicare Advantage plans are offered in specific Service Areas, such as multiple-states, counties, ZIP code areas, or parts of a highly-populated city such as New York or Los Angeles. This means: If you live in Saint Johns County, Florida, you will not have the same selection of Medicare plans as your friends who live in Orange County, California. Our Q1Medicare.com tools are designed to provide people with an overview of all Medicare plan options in their area or region.
(1) Monthly premium. You usually pay a monthly premium for coverage from around $0 to $196 for 2024 stand-alone Prescription drug plans or $0 to $327 for a Medicare Advantage plan that has drug coverage.
(2) Deductible. You may pay an initial deductible where you are 100% responsible for your drug costs before you and your drug plan begin to share the cost of drug coverage (although some drug plans have a $0 deductible and some drug plans with a deductible exclude low-costing generics from the deductible), and
(3) Cost-Sharing. Once you are through your deductible (if any), you and your insurance share the cost of your formulary drugs. For example, you pay 25% of the retail drug price for your medication and your plan pays the remaining 75%, or you pay a flat $2 copay for your generic drugs that retail for $12 and your plan pays the balance.
(4) Limitations on coverage. A Medicare Part D plan (drug insurance) will not cover all medications and each Medicare drug plan can cover different drugs (or drug strengths). So, each year you need to carefully choose a drug plan with a formulary (drug list) that includes your prescriptions - with the knowledge that the formulary can change throughout the plan year (usually substituting newly-released generic drugs for higher-costing brand-name drugs).
(5) Annual drug plan changes. Every year your drug plan can (and usually will) change which drugs the plan covers and the cost associated with the covered drugs. For example, your drug plan may have covered the brand-name drug Lipitor® 10mg for $30, but next year no longer covers Lipitor and instead covers the generic equivalent, Atorvastatin 10mg for $3.
(6) Enrolling into a Medicare Part D drug plan. Just like other types of insurance, there are several ways to enroll into a Medicare drug plan. You can call a Medicare representative at 1-800-Medicare (1-800-633-4227). You can enroll directly though the Medicare plan by calling the plan's toll-free number (usually found on printed plan information or the plan's website. You can enroll through a local insurance agent that represents you chosen Medicare drug plan. You can use a website that represents several Medicare drug plans. For assistance with choosing a Medicare drug plan, you can also call or visit a volunteer such as a SHIP representative or someone at your local senior center.
Question: How do you get Medicare Part D prescription drug coverage?
Your Medicare Part D prescription drug coverage can be provided in several different ways:
- A "stand-alone" Medicare Part D prescription drug plan
(PDP)
A Medicare Part D PDP only provides out-patient prescription coverage and usually does not offer additional or supplemental benefits. You can use our Medicare Part D Plan Finder to review all Medicare Part D plans available in your state: PDP-Finder.com.
- A Medicare Advantage plan that includes prescription coverage
(MAPD)
An MAPD includes your Medicare Part D prescription drug coverage - plus a MAPD includes your Medicare Part A coverage (for in-patient and hospital care) - plus Medicare Part B coverage (for out-patient and physician care) - and often other benefits such as basic dental coverage, optical coverage, hearing aid coverage, and fitness coverage (maybe even transportation coverage, home healthcare, and other supplemental benefits) - all for one monthly premium. Medicare Advantage plans are also called Medicare Part C. You can use our Medicare Advantage plan finder tool to see all Medicare Advantage plans available in your county: MA-Finder.com.
- Finally, you can also receive prescription drug coverage from other sources such as your Union, Employer Health Plan, TRICARE for Life, or the
Veterans Affairs (VA).
A note on employer prescription drug coverage . . . If you are receiving prescription drug coverage from your employer, the key is to ensure that any Employer Health Plan provides "creditable" prescription drug coverage so that you avoid a Late-Enrollment Penalty.
- Medicare Part A - Medicare Part A provides hospital or inpatient coverage.
You may pay a deductible, copayment, or coinsurance (percentage of cost) for care under Medicare Part A. Most people receive Part A without paying a monthly premium because they (or their spouse) have been working (and paying Medicare taxes) for more than 10 years. If you have Medicare Part A, it will be printed on your red, white, and blue Medicare card. Medicare Part A may cover prescription medications during inpatient care.
- Medicare Part B - Medicare Part B provides coverage of doctor visits and out-patient care.
You may pay a deductible, copayment, or coinsurance (percentage of cost) for care under Medicare Part B. You will pay a monthly premium for Medicare Part B coverage (unless you receive some form of financial assistance such as Medicaid). Medicare Part B may pay for some medications that are administered in a doctor's office or by a healthcare provider - but, usually not for self-administered prescriptions. If you have Medicare Part B, it will be printed on your red, white, and blue Medicare card. Medicare Part B should cover vaccinations such as Flu shots.
- Medicare Part C - Medicare Advantage plans are also known as Medicare Part C plans and provide Medicare Part A and Medicare Part B coverage
from private insurance companies.
Medicare Advantage plans can come with prescription drug coverage
(MAPD) or without prescription drug coverage
(MA).
Warning: If you join a Medicare Advantage (MA) HMO or PPO plan (Medicare Advantage plan without drug coverage), you may not be allowed to also join a separate Medicare Part D plan (PDP).
Monthly premiums for Medicare Advantage plan may range from $0 to $327 per month in 2024 - and it is possible that a Medicare Advantage plan will have a monthly premium that is actually less than $0 (the Medicare Advantage plan actually pays you a dividend or rebate on your Medicare Part B premium).
Remember: Medicare Advantage plans are not the same as Medicare Supplements.
- Medicare Part D - Medicare Part D plans provide prescription drug coverage and may be stand-alone Medicare Part D prescription drug plans
(PDP) or Medicare Advantage plans that include prescription drug coverage (MAPD).
Medicare Part D is provided by private insurance companies. Monthly premiums for stand-alone Medicare Part D plans (PDPs) may range from $0 to around $196 per month in 2024.
No. Medicare Part D plans are not required to cover all other prescription drugs - but instead are only required to cover a fixed number of drugs in different therapeutic drug classes. The medications covered by a Medicare Part D plan are organized in a formulary or drug list and this list must cover at least two drugs in each drug category and all drugs (with a few exceptions) in the six therapeutic categories: antidepressants, antispychotics, anticonvulsants (drugs to preventseizures), antiretrovirals (drugs to treat HIV/AIDS), immunosuppressants, and antineoplastics (cancer drugs).
Question: How many different drugs does a Medicare Part D plan cover?
That depends on the drug plan. Each Medicare Part D plan will cover a different number of prescription drugs. In general, a Medicare Part D plan may include several thousand medications in different forms (for instance, 10mg, 20mg, and 40mg Advair Diskus MIS 250/50). Medicare Part D plans also cover vaccinations not covered by Medicare Part B (such as the Shingles Vaccine). Each year, a Medicare drug plan can change the plan's formulary. However, Medicare Part D Medicare Part D plans are regulated by the Centers for Medicare and Medicaid Services (CMS) and CMS must approve a Medicare plan's formulary or drug list every year.
Question: Are any medications excluded from every Medicare Part D plan?
Yes. Some prescription drugs are excluded from the Medicare Part D program by law (such as drugs for weight loss, erectile dysfunction, cosmetic purposes, or hair growth) - however, it is possible that your plan may provide supplemental coverage of these non-Part D drugs as "Bonus Drugs".
Tip: You can see all drugs covered by a particular Medicare plan by using our Q1Medicare Formulary Browser, you can change the name of the Medicare Part D plan and state to browse other formularies. You can also browse all Medicare Part D plans in a certain area that cover a specific medication - and at what cost using our Q1Medicare Drug Finder tool (found at Q1Rx.com).
Question: If I have employer drug coverage can I also join a Medicare Part D drug plan?
Probably not. Warning: If you have an employer health plan that includes prescription drug coverage - and then enroll in a Medicare Part D plan, you risk losing all of your employer health plan coverage, not just drug coverage. You can click here to read more in our Frequently Asked Questions about checking with your employer health plan administrator before enrolling in a Medicare prescription drug plan.
Question: If I have drug coverage through the Veterans Affairs (VA) can I join a Medicare Part D plan?
Yes. If you have VA coverage (that is, prescription drug coverage as part of Veterans Affairs benefits), then you may not need Medicare Part D coverage. However, if you find that the VA does not cover all of your medication needs, you can also enroll in a Medicare Part D program. The two programs cannot be used at the same time for the purchase of a single drug, but actually work together, allowing coordinated coverage - first under the VA and secondly under your Medicare Part D plan. Your VA coverage is also considered "creditable coverage" and should you decide to enroll in a Medicare Part D plan after the close of your initial enrollment period, there will be no penalty for late enrollment. You can click here to read more in our VA section of Frequently Asked Questions.
Question: Am I required to join a Medicare Part D plan?
No. The Medicare Part D program is voluntary and you are not required to enroll in a Medicare Part D plan when you first become eligible for Medicare. However, if you do not have some other form of creditable prescription drug coverage and later decide to join a Part D plan (PDP or MAPD) you may incur a permanent late-enrollment penalty that you will pay in addition to your monthly plan premiums.
Question: How do I enroll into a Medicare Part D plan?
As noted above, there are several ways to join a Part D plan and enrollment depends on your personal preference.
(1) Enroll through a Medicare representative by calling Medicare at 1-800-633-4227 (TTY 1-877-486-2048).Question: If Medicare Part D enrollment is voluntary, what if I don't need drug coverage?
(2) Enroll through a local insurance agent who represents your desired Medicare Part D plan or Medicare Advantage plan.
(3) Enroll with a local volunteer or Senior advocate or Medicare counselor.
(4) Enroll online or over the telephone with an insurance agent who represents multiple Medicare Part D plans or Medicare Advantage plans.
(5) Enroll online through Medicare.gov site (www.medicare.gov/plan-compare/) or a Medicare plan's website.
(6) Submit a printed Medicare plan enrollment application.
For more information on these different enrollment options, please see our FAQ: "How do I enroll in a Medicare Part D or Medicare Advantage plan?"
That depends on you. Choosing a Medicare plan may be somewhat based on your risk tolerance. For instance, people who are not taking any (or only a few generic) medications, can look up the lowest costing Medicare prescription drug plan (or Medicare Advantage plan that includes prescription coverage), check for medication coverage, and decide whether they want to:
- simply enroll in a Medicare plan with the lowest priced monthly premium just to avoid any future
late-enrollment premium penalty or
- pay a little more per month for a Medicare Part D plan with a
$0 deductible and/or a larger formulary and/or a more familiar insurance
company name - just in case their health changes during the plan
year or
- join a Medicare Advantage plan that includes drug coverage
(MAPD) has a $0 (or low) monthly premium and a healthcare network that
includes many local doctors and other healthcare providers or
- skip enrolling in any Medicare Part D plan this year, save
the monthly premiums, and plan to pay the late-enrollment penalty if
they ever choose to join a Medicare Part D or Medicare Advantage plan in
the future.
Warning: Yes, the monthly penalties can add up and here is a chart showing how your penalty costs can increase over time: Q1FAQ.com/590
People with more complex medication or healthcare needs must spend more time ensuring that their specific needs (medical and prescription drugs) are covered by a Medicare Part D or Medicare Advantage plan. For example, if you have a particular plan in mind (such as a local Medicare Advantage HMO POS that is provided by the large university or hospital system in your area), then you can review all of the coverage details we have online - and then call the plan to learn whether their healthcare providers are included in the Medicare Advantage plan's network.
Question: If I don't join a drug plan when I am first eligible, how is the Late-Enrollment Penalty calculated?
Late-Enrollment Penalties are assessed when you eligible for Medicare Part D coverage, but are without some form of creditable drug coverage for more than 63 days. You can click here to read more in our late-enrollment premium penalty section of Frequently Asked Questions. Late-enrollment penalties are permanent and can change (increase) year-to-year. You will pay 1% of the national base Medicare Part D premium $34.70 in 2024) for every month that you were without some creditable prescription drug coverage before you enrolled in a Medicare Part D plan. So if you were eligible for Medicare when you were 65 and now you are 70, you would pay a penalty based on 60 months without coverage (5 years * 12) or about 60% of the annual base premium (so around $34.70 * .6 = $20.80 per month in addition to your monthly Part D plan premium).
Question: Are all Medicare Part D plans about the same and available everywhere?
No. Medicare Part D coverage will vary plan-to-plan and not all Medicare plans are available in all areas of the country. Remember: Medicare Part D and Medicare Advantage plans are offered in specific Service Areas, such as multiple-states, counties, ZIP code areas, or parts of a highly-populated city such as New York or Los Angeles. This means: If you live in Saint Johns County, Florida, you will not have the same selection of Medicare plans as your friends who live in Orange County, California. Our Q1Medicare.com tools are designed to provide people with an overview of all Medicare plan options in their area or region.
Question: How does a Medicare Part D plan actually work?
Your Medicare Part D plan is divided into four (4) parts or phases of coverage.
(1) The Initial Deductible is when you pay 100% of your retail drug costs until you reach your deductible amount (for instance, the 2024 standard initial deductible is $545 ($590 in 2025). Many people will enroll in a Medicare prescription drug plan with a $0 deductible and effectively skip-over this first "deductible" phase. Also, some Medicare Part D plans will exclude less-expensive drugs (such as Tier 1 generics) from the plan's initial deductible, so it is possible that you may have coverage for some low-costing drugs even though you have not met your plan's initial deductible. Once you meet your plans Initial Deductible (if any), then you move to the next part of your coverage: the Initial Coverage Phase.
(2) The Initial Coverage phase is when you and your Medicare Part D plan will share in the cost of your medication purchases based on your plan's cost-sharing (such as a $30 copayment or 25% coinsurance). When the retail value of your drug purchases exceeds your Initial Coverage Limit (ICL or Donut Hole entry point), you will leave your Initial Coverage Phase and enter the Coverage Gap or Donut Hole. Most people will never leave their Initial Coverage Phase during the plan year.
Please note that the Initial Coverage Limit is not measured by what you have spent on medications. Instead, the ICL is the total retail value of your prescription drug purchases. So, the ICL is the amount that you pay for your prescriptions plus what your Medicare Part D plan is paying. The 2024 ICL is $5,030. The ICL will no longer exist in 2025 -- see below.
For example, if you fill a $100 prescription in 2024 and you pay a $30 copay (the Medicare Part D plan pays the other $70), the total $100 retail cost is counted toward your 2024 Initial Coverage Limit of $5,030. In this case, after the $100 drug purchase, you have $4,930 remaining in drug purchases before entering the 2024 Donut Hole or Coverage Gap.
(3) The Coverage Gap or Donut Hole is the drug plan phase you enter once you exceed the Initial Coverage Limit and you receive a Donut Hole Discount or 75% discount on formulary drugs (you will pay 25% of your plan's negotiated retail cost).
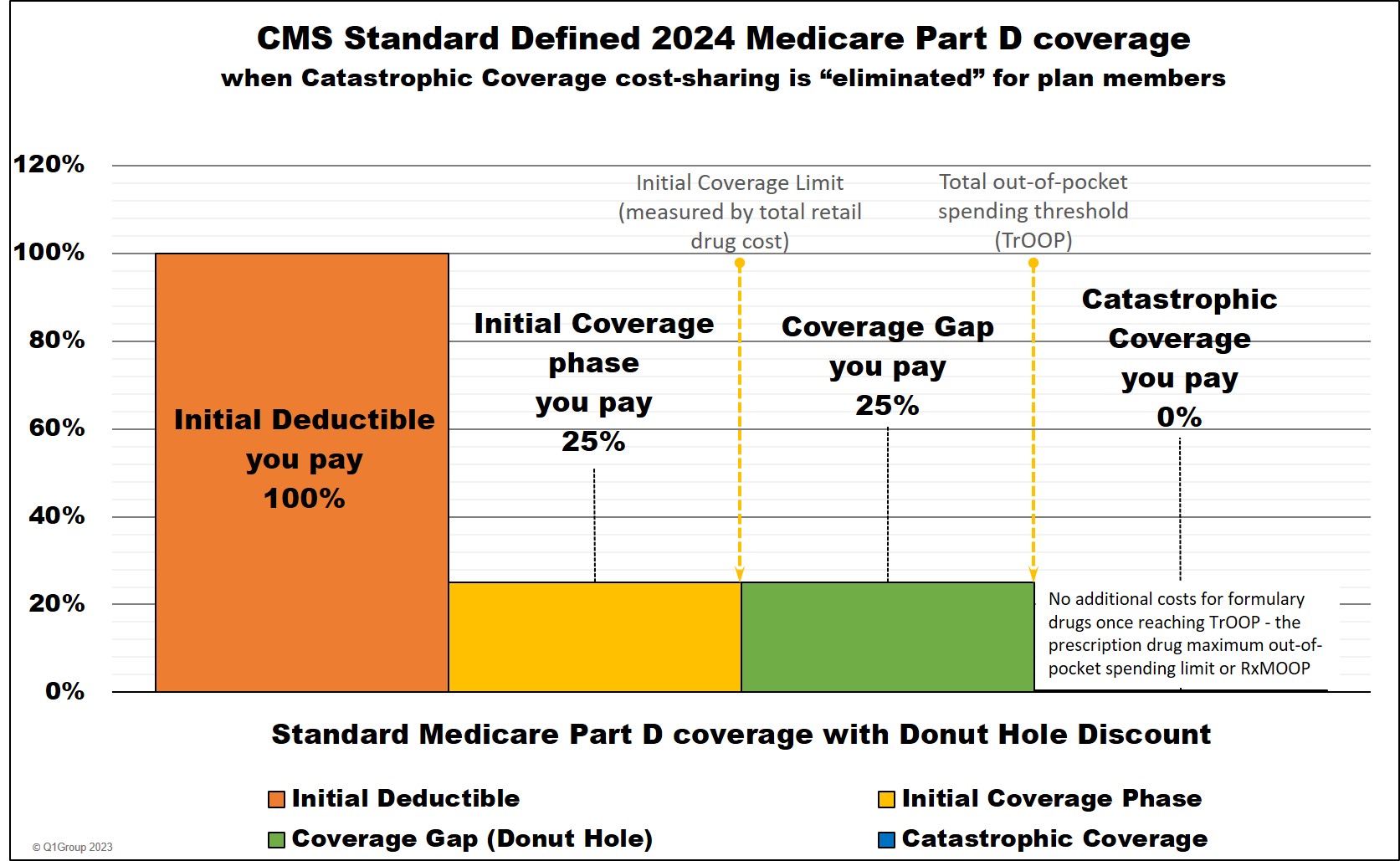
Important Fact: 2024 is the last year that the Donut Hole will exist.
In 2025 one of the provisions of the Inflation Reduction Act (IRA) of 2022 is the elimination of the Coverage Gap (Donut Hole). Medicare Part D beneficiaries will stay in the Initial Coverage phase until they reach the maximum cap on out-of-pocket spending for Part D formulary drugs - RxMOOP - which is set at $2,000 for 2025. After reaching RxMOOP Medicare Part D beneficiaries will enter the Catastrophic Coverage Phase.
(4) The Catastrophic Coverage Phase is the last phase of your Medicare Part D plan coverage and you enter once your total out-of-pocket drug costs (TrOOP) exceed a certain point (RxMOOP) which is $8,000 in 2024 and $2,000 in 2025. During this phase you will pay nothing ($0) for your formulary drug purchases for the remainder of the year.
TrOOP is what you have spent out of pocket for medications, but does not include your monthly premiums. Also, although you receive a 75% discount on brand-name drugs in the Donut Hole (you pay 25% of retail), you will actually get 95% of the retail price credited toward your TrOOP.
So, if you purchase a brand-name drug in the Donut Hole with a retail cost of $100, you pay $25 (you get a 75% discount) and you get $95 credited toward your TrOOP or Donut Hole exit point. (Please note: this is a good thing because you will need to spend less to get out of the Donut Hole phase and enter the lower-costing Catastrophic Coverage phase.)
Keep in mind that 2023 was the last year that Medicare Part D beneficiaries will pay cost-sharing in the Catastrophic Coverage phase. For plan year 2024, the Inflation Reduction Act (IRA) of 2022 eliminates beneficiary cost-sharing in the Catastrophic Coverage phase.
Question: When can I enroll in a Medicare Part D plan?
Your Initial Enrollment Period (IEP)
If you are new to Medicare, you have an Initial Enrollment Period (IEP) that is a seven (7) month window beginning three (3) months before your month of eligibility, plus the month of eligibility, and ends three (3) months after your month of eligibility.
If you enroll in the three months prior to your month of Medicare eligibility, your effective date (when your plan coverage begins) is the 1st day of your month of Medicare eligibility.
If you enroll in a Medicare Part D plan during your month of eligibility (such as when you turn 65) or during the three months following the month of Medicare eligibility, your Medicare Part D plan will be effective on the 1st day of the month following receipt of your plan enrollment.
The annual Open Enrollment Period (AEP)
If you are already eligible for Medicare, you can change Medicare plans during the Annual Open Enrollment Period (AEP). The Annual Enrollment Period starts each year on October 15th and continues through December 7th with your Medicare Part D plan becoming effective on January 1st of the new plan year. This time period can also be called the annual Open Enrollment Period -- which is still referred to as "AEP".
Special Enrollment Periods (SEPs)
If you are outside of your IEP or AEP, then you will need to use a Special Enrollment Period (SEP) to change Medicare Part D or Medicare Advantage plans. An SEP may be granted when you move outside of your plan's Service Area (move to another state) or move into an assisted living facility or when you qualify for Extra Help.
If you are entitled to an SEP, your Medicare Part D plan will become effective on 1st day of the month following the receipt of your enrollment. See our Special Enrollment Period FAQ for more details and examples of SEPs.
Question: What do you pay for your Medicare plan coverage?
(1) Your monthly premium
As noted above, if you join a Medicare Part D prescription drug plan (PDP), you will pay a monthly premium ranging from only a few dollars up to over 100 dollars. If you join a Medicare Advantage plan (MA or MAPD), you may have a $0 premium - and, depending on the MAPD, may actually get a portion of your Medicare Part B premium rebated back to you (a "dividend" plan). Your monthly premiums will vary depending on the benefits of your selected Medicare Part D plan or Medicare Advantage plan and your resident state.
You can see a list of all Medicare Part D plans in your state using our Medicare Part D Plan Finder (PDP-Finder.com/FL). You can see a list of all Medicare Advantage plan in your ZIP code using our Medicare Advantage Plan Finder (MA-Finder.com/90210). You can also learn about the Medicare Part D plan premiums in your area by calling Medicare at 1-800-633-4227.
(2) Your prescription drug costs
As mentioned, your coverage costs can change depending on the phases of your Medicare Part D plan. In the Initial Deductible, you will pay 100% of your retail drug costs. In the Initial Coverage phase, you will share the cost with your drug plan (for example, you pay 25% of retail or a fixed copay of $30 for brand-name drugs). In the 2024 Coverage Gap or Donut Hole, you will receive a 75% discount on all formulary drugs. In the Catastrophic Coverage phase, you will pay nothing for your medications.
(3) Your healthcare costs - with a Medicare Advantage plan.
If you join a Medicare Advantage plan that includes drug coverage (MAPD), you will receive coverage as mentioned above and you will also receive coverage for your Medicare Part A (in-patient costs) and Medicare Part B (out-patient costs), plus you may also receive additional dental, vision, health club coverage, depending on your plan. The Medicare Advantage plan coverage should be at least as good as the Original Medicare coverage provided by the government. However, Medicare Advantage plans will have a maximum out-of-pocket spending limit (MOOP), that will be around $8,850 in 2024 or less - meaning that your healthcare costs will not exceed this amount for a calendar year.
Question: Is there financial assistance to help me pay my Medicare Part D prescription drug costs - and Medicare Part A or Medicare Part B costs?
Yes. The Medicare Part D Extra Help program is available to help people with limited financial resources pay for their monthly premiums and drug costs. The Extra Help or Low-Income Subsidy (LIS) program is based on a Medicare beneficiary’s income and assets (financial resources). For more information, please contact your state Medicaid office.
Medicare Savings Programs are also available and, depending on your finances, may help pay Medicare Part A and/or Medicare Part B premiums, and maybe some Medicare Part B costs.
Question: Can a Medicare Part D plan change every year?
Yes. Important: Please note that Medicare Part D and Medicare Advantage plans change each year. For example, if you are eligible for Medicare in 2024, the Medicare Part D plans that you review in 2023 or 2022, may not be available to you in 2024. If you find that a Medicare plan is available next year, the plans can (and probably will) have different costs, coverage, and healthcare providers. As an example, this graph shows the changing Medicare Part D plan parameters since the beginning of the Medicare Part D program.
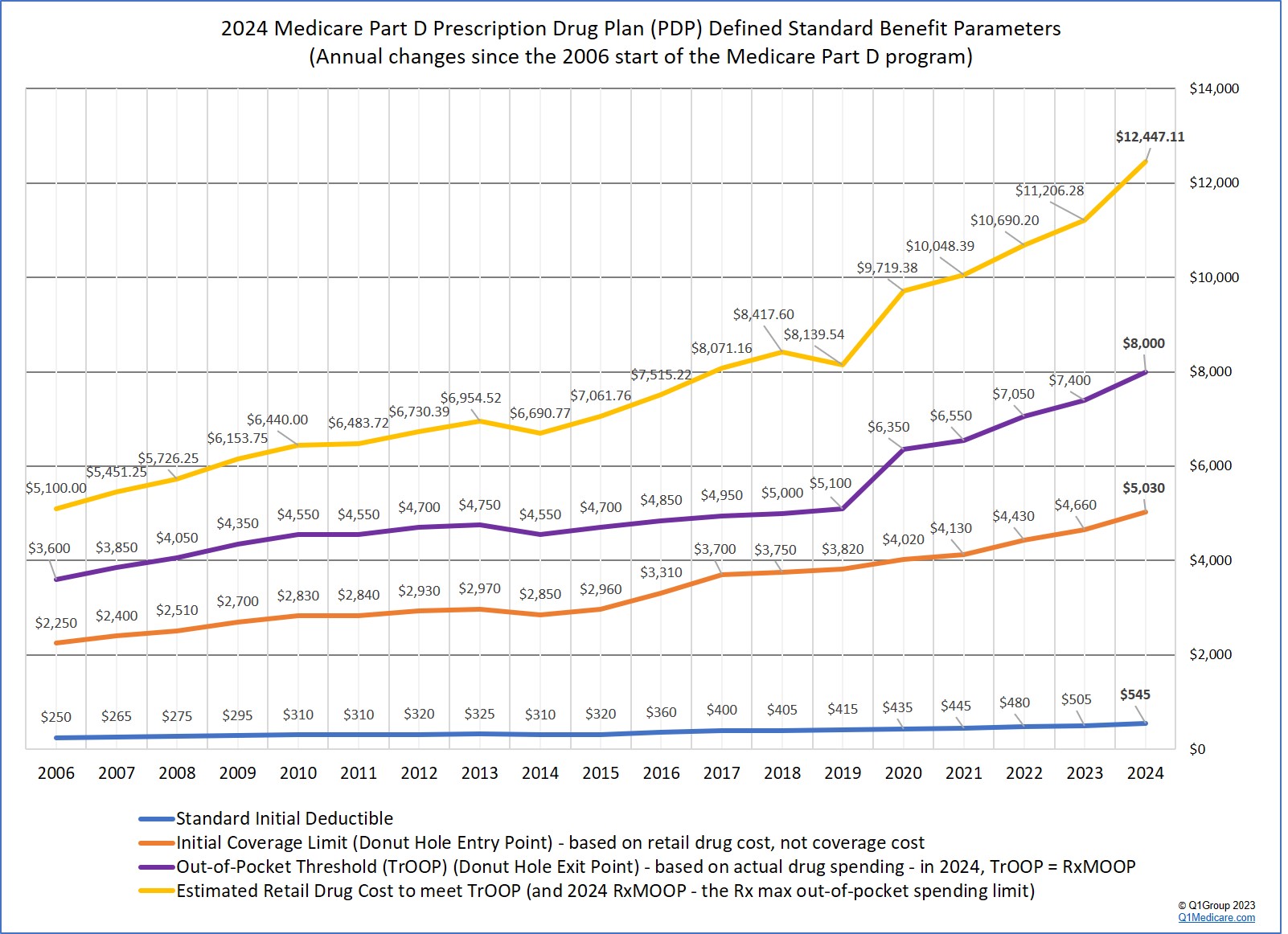
Bottom Line: Be prepared to review your Medicare plan options each year to ensure the most economic and complete coverage.
Question: How do we choose a Medicare Part D or Medicare Advantage plan?
There is no one "right" way to choose a Medicare Part D or Medicare Advantage plan. In general, we simply advise people to choose a Medicare plan that most economically covers their current health and prescription needs. The Centers for Medicare and Medicaid Services (1-800-Medicare) suggest that you look at the factors of Coverage, Cost, and Convenience - to these criteria we also add that you should probably consider the Company and your level of Comfort.
Need a place to begin?
To get started, you can begin on our homepage (Q1Medicare.com) and see the box that is entitled "2024 Medicare Part D plans" with a listing of state abbreviations for stand-alone Medicare Part D prescription drug plans. For example, if you live in the Commonwealth of Virginia, choose "VA", you will be taken to an overview of all Medicare Part D prescription drug plans in Virginia: PDP-Finder.com/VA
On this page, you can see the name of the Medicare Part D plans, the monthly premium, the initial deductible, and the copayment rate for the different drug tiers.
Browsing a plan's formulary or drug list
If you wish to see the medications covered by this Medicare Part D plan, you can click on the "Browse Formulary" link on the right side of the chart to use our Formulary-Browser.com. You can also click on the icons under the plan names for more plan details and plan contact information.
An example of using the Formulary Browser
Here is an example link to the first page of the Humana Walmart Value Rx Plan formulary in Virginia.
(Important: when browsing a plan formulary or other healthcare coverage information, be sure you are looking at formulary or Medicare plan information for the current enrollment year - the plan year should be printed on the plan documents or shown on the computer screen.)
From this Humana Walmart Rx Plan example link, you can see the medication names and packaging information, drug tier number, tier description, cost-sharing and usage management restrictions (if any). Using our Formulary Browser, you can always change the name of the Medicare Part D plan and state to browse other formularies.
Using the Q1Rx Drug Finder tool to see how all plans in your area cover a particular drug
You can also click on the icon after the drug name and you can see all of the Medicare Part D plans in Virginia that also cover this same medication and at what cost. (This is our Drug Finder tool (found at Q1Rx.com) and you can change the prescription name to whatever you wish.)
Finding a Medicare Advantage plan in your ZIP code
If you are looking for a Medicare Advantage plan (with Medicare Part A, Medicare Part B, and possibly Medicare Part D coverage), you can start on the Q1Medicare homepage and see the box with the titled "2024 Medicare Advantage Plans". You can then enter your ZIP code or click on your state (and then county) to see the Medicare Advantage plans available in your chosen location. (Medicare Part D plans are available state-wide, Medicare Advantage plans are offered on a ZIP code or county area or partial-county.)
An example of the Medicare Advantage plan finder
As an example, here are the Medicare Advantage plans available in Fairfax County, Virginia:
MAFinder.com/22124
Again, you can see the basic coverage details of all these Medicare Advantage plans in the list, along with Medicare Part D prescription drug coverage details, if included on the plan (or MAPD). The icon below the Medicare Advantage plan name that looks like a small stack of paper will show all of the coverage details for a specific Medicare Advantage plan.
Still need more help with specific issues? Browse our Frequently Asked Questions
If you have specific questions, you can always browse our FAQ section found here: Q1FAQ.com
The Medicare & You Handbook online with additional information
We also have the CMS Medicare & You Handbook online, alone with our supplemental notes and information: q1medicare.com/PartD-MedicareAndYouCMSGuideToMedicare.php
When you need to speak with someone about your plan options or are ready to enroll . . .
If you feel lost or overwhelmed along the way, you can always contact Medicare directly at 1-800-633-4227 (1-800-Medicare), select the prescription drug option, and then choose the option to speak with a Medicare representative or say "representative" during the menu options.
Once connected, you can explain your situation to a Medicare representative and ask them to help you find a Medicare Advantage plan or Medicare Part D prescription drug plan that most economically covers your health and medication needs - or you can ask specific questions about a particular Medicare plan or the Medicare Part D program in general.
If you find a suitable Medicare Advantage plan or Medicare Part D plan and are eligible to enroll in the plan, the Medicare representative can process your enrollment in your chosen Medicare plan directly over the telephone - and the process only takes a few minutes. A Medicare representative is not compensated for a Medicare plan enrollment and provides you with an unbiased view of all available Medicare Part D plans or Medicare Advantage plans.
There is no one "right" way to choose a Medicare Part D or Medicare Advantage plan. In general, we simply advise people to choose a Medicare plan that most economically covers their current health and prescription needs. The Centers for Medicare and Medicaid Services (1-800-Medicare) suggest that you look at the factors of Coverage, Cost, and Convenience - to these criteria we also add that you should probably consider the Company and your level of Comfort.
- Coverage - Ask yourself: Are your prescription medications covered by this
plan? Are there low-costing generic alternatives for your brand-name drugs? Can
you work with this plan to get a
formulary exception should you need a
medication that is not covered on the existing formulary? How large (generous) is the Part D plan's formulary or drug list? What
formulary price-tiers apply to your medications ($30 copay or 33% of retail)? What health coverage does the
Medicare Advantage plan offer beyond basic Medicare? What is the Medicare Advantage plan's maximum out-of-pocket limit (MOOP)? Are there any
additional coverage benefits offered by the plan?
- Cost - What are the monthly plan premiums? Does the Medicare
Part D plan or Medicare Advantage plan have an initial deductible?
Are there any drug tiers excluded from the deductible that would provide immediate coverage? What are the copayments or coinsurance that you pay for your
medications or healthcare? What are the plan's coverage limits? Is
there any prescription coverage in the Donut Hole beyond the Donut Hole discount?
- Convenience - How difficult is it to find a pharmacy or a
health care provider? (Note: most Medicare Part D plans now have a
pharmacy network of 50,000 to over 65,000+ pharmacies.) Does the Medicare Advantage plan have a restricted healthcare network? Do your doctors (hospitals) accept this Medicare Advantage
plan? How easy is it to work with this Medicare Part D plan or Medicare
Advantage plan when it comes to asking for Prior Authorization or exceptions to
utilization management restrictions?
- Company - Is the company who provides the Medicare Part D or
Medicare Advantage plan important to you? Often people choose a
Medicare plan based only the Medicare plan provider's reputation or
recommendation. Does the company have an acceptable
quality star rating?
- Comfort - Are you comfortable with your current Medicare Part
D plan or Medicare Advantage plan? If you could find a more affordable Medicare plan, would you rather spend a few extra
dollars per month because you have an idea how your current Medicare
plan operates - and your plan costs are predictable - and you know that you can work with the plan? (Tip: If you are suggesting that your parents or friends change Medicare plan coverage based on pure economics, be sure to understand your parent's (or friends') level of comfort with their existing plan (doctors, pharmacists, specialists) - before persuading them to change Medicare plans.)
Still looking for more? Here are some general tips specifically for Medicare Part D prescription drug plan selection: Choosing a Plan: The Basics
Need a place to begin?
To get started, you can begin on our homepage (Q1Medicare.com) and see the box that is entitled "2024 Medicare Part D plans" with a listing of state abbreviations for stand-alone Medicare Part D prescription drug plans. For example, if you live in the Commonwealth of Virginia, choose "VA", you will be taken to an overview of all Medicare Part D prescription drug plans in Virginia: PDP-Finder.com/VA
On this page, you can see the name of the Medicare Part D plans, the monthly premium, the initial deductible, and the copayment rate for the different drug tiers.
Browsing a plan's formulary or drug list
If you wish to see the medications covered by this Medicare Part D plan, you can click on the "Browse Formulary" link on the right side of the chart to use our Formulary-Browser.com. You can also click on the icons under the plan names for more plan details and plan contact information.
An example of using the Formulary Browser
Here is an example link to the first page of the Humana Walmart Value Rx Plan formulary in Virginia.
(Important: when browsing a plan formulary or other healthcare coverage information, be sure you are looking at formulary or Medicare plan information for the current enrollment year - the plan year should be printed on the plan documents or shown on the computer screen.)
From this Humana Walmart Rx Plan example link, you can see the medication names and packaging information, drug tier number, tier description, cost-sharing and usage management restrictions (if any). Using our Formulary Browser, you can always change the name of the Medicare Part D plan and state to browse other formularies.
Using the Q1Rx Drug Finder tool to see how all plans in your area cover a particular drug
You can also click on the icon after the drug name and you can see all of the Medicare Part D plans in Virginia that also cover this same medication and at what cost. (This is our Drug Finder tool (found at Q1Rx.com) and you can change the prescription name to whatever you wish.)
Finding a Medicare Advantage plan in your ZIP code
If you are looking for a Medicare Advantage plan (with Medicare Part A, Medicare Part B, and possibly Medicare Part D coverage), you can start on the Q1Medicare homepage and see the box with the titled "2024 Medicare Advantage Plans". You can then enter your ZIP code or click on your state (and then county) to see the Medicare Advantage plans available in your chosen location. (Medicare Part D plans are available state-wide, Medicare Advantage plans are offered on a ZIP code or county area or partial-county.)
An example of the Medicare Advantage plan finder
As an example, here are the Medicare Advantage plans available in Fairfax County, Virginia:
MAFinder.com/22124
Again, you can see the basic coverage details of all these Medicare Advantage plans in the list, along with Medicare Part D prescription drug coverage details, if included on the plan (or MAPD). The icon below the Medicare Advantage plan name that looks like a small stack of paper will show all of the coverage details for a specific Medicare Advantage plan.
Still need more help with specific issues? Browse our Frequently Asked Questions
If you have specific questions, you can always browse our FAQ section found here: Q1FAQ.com
The Medicare & You Handbook online with additional information
We also have the CMS Medicare & You Handbook online, alone with our supplemental notes and information: q1medicare.com/PartD-MedicareAndYouCMSGuideToMedicare.php
When you need to speak with someone about your plan options or are ready to enroll . . .
If you feel lost or overwhelmed along the way, you can always contact Medicare directly at 1-800-633-4227 (1-800-Medicare), select the prescription drug option, and then choose the option to speak with a Medicare representative or say "representative" during the menu options.
Once connected, you can explain your situation to a Medicare representative and ask them to help you find a Medicare Advantage plan or Medicare Part D prescription drug plan that most economically covers your health and medication needs - or you can ask specific questions about a particular Medicare plan or the Medicare Part D program in general.
If you find a suitable Medicare Advantage plan or Medicare Part D plan and are eligible to enroll in the plan, the Medicare representative can process your enrollment in your chosen Medicare plan directly over the telephone - and the process only takes a few minutes. A Medicare representative is not compensated for a Medicare plan enrollment and provides you with an unbiased view of all available Medicare Part D plans or Medicare Advantage plans.
Browse FAQ Categories
Pets are Family Too!
Use your drug discount card to save on medications for the entire family ‐ including your pets.
- No enrollment fee and no limits on usage
- Everyone in your household can use the same card, including your pets
Your drug discount card is available to you at no cost.
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
